Genetic Breakthrough Identifies Heart Failure Risk in African and Latino Americans
Findings may inform genetic screening test for patients at risk and medically under-served
A genetic variation believed to increase risk for heart failure in people of African or Latino ancestry has been identified in a new study by researchers from the Icahn School of Medicine at Mount Sinai and Perelman School of Medicine at the University of Pennsylvania.
The study found that the transthyretin or TTR V122I genetic variant was significantly associated with heart failure and that heredity transthyretin amyloid cardiomyopathy (hATTR-CM) caused by this variant was confirmed at appreciable frequency in individuals of African or Latino ancestry. The results suggest a significant under-recognition and under-diagnosis of this potentially fatal disease.
The results of the study were published today in JAMA.
hATTR-CM causes deposits of abnormal proteins called amyloids in the heart, nerves, and sometimes the kidneys and other organs, resulting in progressive organ dysfunction. The condition can run in families. Symptoms may start as early as age 20 or as late as age 80, and the average delay in diagnosis is four years. Treatment was limited to supportive care until May of this year, when the Food and Drug Administration approved tafamidis, the first and only targeted TTR therapy. Even with this new treatment, timely diagnosis is key, as the medication can only delay disease progression, not reverse the symptoms.
“Given recent advances in treatment for hATTR-CM, it is imperative to identify patients at risk for the disease and intervene before noticeable symptoms of the disease appear,” said study author Ron Do, PhD, Assistant Professor of Genetics and Genomics Sciences, and co-Director of the BioMe Phenomics Center in The Charles Bronfman Institute for Personalized Medicine at the Icahn School of Medicine at Mount Sinai. “Previous studies have proposed utilizing routine genetic testing for individuals with African ancestry; however, this is not current practice and the scope of the under-diagnosis is not clear.”
In this observational study, the association of the TTR V122I variant with the clinical diagnosis of heart failure was evaluated using longitudinal electronic health record-linked genetic data from two large integrated academic health systems, the Icahn School of Medicine at Mount Sinai BioMe biobank (BioMe) and the Penn Medicine Biobank (PMBB). Among carriers of the TTR V122I variant, the rates of evaluation for and diagnosis with hATTR-CM was assessed.
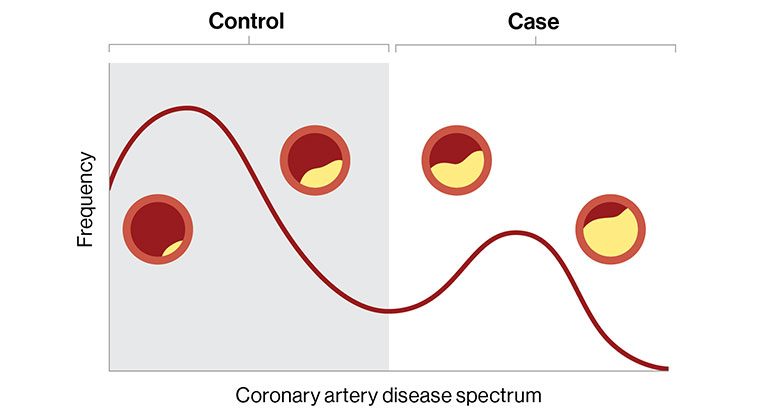
Because the TTR V122I variant predominantly occurs in individuals of African ancestry, researchers analyzed the association between TTR V122I variant carrier status and heart failure in 9,694 individuals of African (BioMe and PMBB) and Latino (BioMe) ancestry enrolled in one of the two biobanks. In PMBB, a cross-sectional analysis was performed, comparing the rate of heart failure between TTR V122I variant carriers and non-carriers in individuals of genetically inferred African ancestry aged 50 years or older. The analysis in BioMe used a case-control design among individuals of self-reported African or Latino ancestry, comparing the number of TTR V122I carriers and non-carriers between all participants with prevalent heart failure cases and individuals over the age of 65 without heart failure.
Patients of African or Latino ancestry with TTR V122I genetic variant are two-fold more likely to have heart failure risk. Across both study samples, researchers also observed left-ventricular-wall thickening, which could be a sign of early subclinical heart failure. Higher rates of left-ventricular-wall thickening among younger TTR V122I carriers without overt heart failure were detected in the BioMe cohort, suggesting subtle changes in the heart may develop years prior to the onset of advanced signs and symptoms of the disease. Finally, only 11 percent of individuals with the genetic variant and heart failure were diagnosed with transthyretin cardiomyopathy, with an average time to diagnosis of three years, indicating both high rates of underdiagnosis and prolonged time to appropriate diagnosis.
“These findings suggest that although the TTR genetic variant is known to cause hereditary TTR amyloidosis cardiomyopathy and heart failure, there is significant under-recognition and under-diagnosis of this disease, particularly in individuals of African and/or Latino ancestry,” said study co-author Girish Nadkarni, MD, Assistant Professor of Medicine (Nephrology) and co-Director of the BioMe Phenomics Center in The Charles Bronfman Institute for Personalized Medicine at the Icahn School of Medicine at Mount Sinai. “Of the observed cases, only 11 percent of individuals with the TTR genetic variant were diagnosed appropriately. It’s imperative that genetic screening of TTR genetic variants be considered for early diagnosis of the disease and its treatment.”
Mount Sinai authors of the study include Kumardeep Chaudhary, PhD; Judy H. Cho, MD; Edgar Argulian, MD; Lili Chan, MD; Amanda Dobbyn, PhD; Aparna Saha, MD; Tielman Van Vleck, MD; Noura S. Abul-Husn, MD; Eimear E. Kenny, PhD; Ruth J. Loos, PhD; and Jagat Narula, MD, PhD.
Perelman School of Medicine at the University of Pennsylvania authors include Daniel J. Rader, MD (corresponding author); Scott M. Damrauer, MD; Lusha W. Liang, MD; Marie A. Guerraty, MD, PhD; Renae Judy, MS; Jenna Kay, MD; Rachel L. Kember, PhD; Michael G. Levin, MD; Shefali S. Verma, PhD; Julio A. Chirinos, MD; JoEllen Weaver, BS; Brian Drachman, MD; Marylyn Ritchie, PhD.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, employing 48,000 people across its hospitals and more than 400 outpatient practices, as well as more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
Digital Marker for Coronary Artery Disease Built by Researchers at Mount Sinai
Dec 20, 2022 View All Press Releases
Most “Pathogenic” Genetic Variants Have a Low Risk of Causing Disease
Jan 25, 2022 View All Press Releases