Blacks Found Twice as Likely to Have Atherosclerosis as Hispanics in Young Adult Populations in Underserved Communities
Mount Sinai study emphasizes importance of early screening and lifestyle interventions to prevent adverse cardiac events
A unique Mount Sinai study focused on a multi-ethnic, underserved community in New York City shows that young Black adults are twice as likely to have atherosclerosis as similarly situated young Hispanic adults.
Atherosclerosis is plaque build-up in the arteries that can lead to a blockage, causing a heart attack or stroke. The research, published July 11 in the Journal of the American College of Cardiology, is one of the first to evaluate atherosclerotic plaque in asymptomatic young urban populations and emphasizes the importance of early screening and lifestyle interventions in high-risk minority groups to improve their cardiovascular health.
“What’s interesting about this study is that Black individuals appear to be more vulnerable to atherosclerosis early in life than people of Hispanic origin, even when adjusting for known cardiovascular and lifestyle risk factors such as smoking, unhealthy diet, lack of exercise, high blood pressure, and cholesterol. This can then put them at increased risk of cardiovascular disease, suggesting the existence of emerging or undiscovered cardiovascular risk factors in this population,” says Valentin Fuster, MD, PhD, Director of Mount Sinai Heart and Physician-in-Chief of The Mount Sinai Hospital, who created and led the trial, called the FAMILIA Project at Mount Sinai Heart.
The study is part of an ambitious multinational effort to intervene early in the lives of children, their caretakers, and teachers so they can form a lifetime of heart-healthy habits. These new results come after highly successful interventions involving more than 500 pre-schoolers, caretakers, and educators at 15 Head Start schools in the Harlem section of Manhattan, an urban area that is socioeconomically disadvantaged—a situation commonly linked to higher rates of obesity, heart disease, and other health issues.
The FAMILIA team focused on 436 adults, including pre-schoolers’ family members, caretakers, teachers, and school staff. Of that group, 147 participants were Black and 289 were Hispanic, with an average age of 38; 80 percent were women. Each one answered a comprehensive questionnaire at the start of the study, addressing their nutrition, physical activity, tobacco use, alcohol consumption, and whether they had conditions such as heart disease, hypertension, diabetes, or a family history of health problems. They also had their weight recorded, and blood pressure and cholesterol checked.
Overall cardiovascular risk factors were prevalent for both ethnic groups at baseline. Thirty percent of Black participants had hypertension, almost triple the rate of the Hispanic group, 11 percent. Conversely, Black participants had lower rates of dyslipidemia—unhealthy levels of lipids/fat in the blood (18 percent) compared to the Hispanic group at 27 percent, and better eating habits, consuming more fruits and vegetables. Researchers used this data to calculate a predicted cardiovascular risk score for each group. They found the overall risk of having a cardiovascular event in 10 years was low for both Blacks and Hispanics—around four percent for both groups.
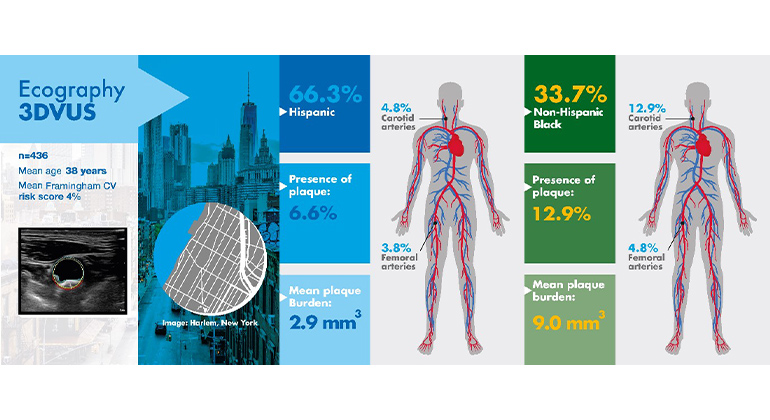
Participants also had 3D vascular ultrasounds to determine if they had atherosclerosis in their carotid (neck) and femoral (leg) arteries. These vascular ultrasounds pointed to a significant discrepancy between the groups. Overall, nine percent of participants had subclinical atherosclerosis (nearly one in ten participants showed at least one artery with plaque). Also, the rate of plaque build-up in the arteries was two times higher among Blacks than Hispanics. The results were consistent even after adjusting for classic cardiovascular risk factors including age, sex, body mass index, hypertension, diabetes, and cholesterol; lifestyle factors including diet, physical activity, and tobacco use; and socioeconomic factors such as employment status.
“These findings may in part help to explain the observed differences in cardiovascular disease prevalence between racial and ethnic groups,” Dr. Fuster adds. “The study further contributes to the understanding of higher rates of cardiovascular disease observed at an early age in disadvantaged communities. Until underlying biological factors and other undiscovered cardiovascular risk factors are better understood and can be addressed by precision medicine, affordable noninvasive imaging techniques such as the portable 3D vascular ultrasounds used in this study, which are easily used and affordable, can be an important form of early detection in underserved communities, and provide valuable information about population disparities and increase the precision of health promotion and prevention programs.”
Dr. Fuster and his team will expand the FAMILIA program to schools across the five boroughs of New York City starting in September 2022. This project will also evaluate how family socioeconomic status and teachers’ characteristics may affect the implementation and efficacy of school-based health promotion programs.
The FAMILIA project was funded by a grant from the American Heart Association.
Figure: Subclinical Atherosclerosis in Hispanic and Non-Hispanic Black Socioeconomically Vulnerable Young Adults
Description: This study assessed the impact of race and ethnicity on early subclinical atherosclerosis, as assessed by bilateral carotid and femoral 3DVUS, on 436 young Hispanic and non-Hispanic Black adults (parents/caregivers and staff) recruited in the FAMILIA trial from 15 Head Start preschools in Harlem (New York City). After adjustment for traditional CV risk, lifestyle, and socioeconomic factors, non-Hispanic Black individuals were more likely than Hispanic individuals to have subclinical atherosclerosis and higher burden of disease, suggesting the existence of unknown cardiovascular risk factors underlying such residual excess risk. Early detection of atherosclerosis could play an important role in prevention programs in different populations.
Mount Sinai Heart is one of the nation’s top 6 hospitals in Cardiology/Heart Surgery
Mount Sinai Heart is among the top 6 in the nation for cardiology and cardiac surgery according U.S. News & World Report. Newsweek’s “The World’s Best Specialized Hospitals” ranks Mount Sinai Heart as No. 1 in New York and No. 4 globally.
It is part of Mount Sinai Health System, which is New York City's largest academic medical system, encompassing eight hospitals, a leading medical school, and a vast network of ambulatory practices throughout the greater New York region. We advance medicine and health through unrivaled education and translational research and discovery to deliver care that is the safest, highest-quality, most accessible and equitable, and the best value of any health system in the nation. The Health System includes approximately 7,300 primary and specialty care physicians; 13 free-standing joint-venture centers; more than 410 ambulatory practices throughout the five boroughs of New York City, Westchester, and Long Island; and more than 30 affiliated community health centers. The Mount Sinai Hospital is ranked in U.S. News & World Report's "Honor Roll" of the top 20 U.S. hospitals and among the top in the nation by specialty: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Urology, and Rehabilitation. For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.

Valentin Fuster, MD, PhD, Receives Prestigious Award from City of Barcelona, Spain
Jan 23, 2023 View All Press Releases
Samin Sharma, MD, Named Director of the Mount Sinai Cardiovascular Clinical Institute
Nov 28, 2022 View All Press Releases
Valentin Fuster, MD, PhD, Named President of Mount Sinai Heart
Oct 18, 2022 View All Press ReleasesThe Mount Sinai Hospital Awarded Highest Quality Rating for Adult Cardiac Valve Surgery
May 28, 2019 View All Press Releases