Brain’s Sensitivity to Different Types of Regret May Impact Mood Disorders Like Depression, Mount Sinai Researchers Find
Researchers from the Icahn School of Medicine at Mount Sinai have learned that the way the brain processes the complex emotion of regret may be linked to an individual’s ability to cope with stress, and altered in psychiatric disorders like depression.
The study, published October 19 in Science Advances, reveals that mice show sensitivity to two distinct types of regret and that these different thought processes likely stem from different parts of the brain. The team also discovered that a genetic marker that predisposes maladaptive stress response traits and vulnerability to depression was linked to sensitivity to one type of regret whereas healthy and stress-resilient animals were instead sensitive to a second type of regret.
These novel findings could have broad implications for multiple fields, including psychiatry, psychology, and behavioral economics, and could inform the future design of targeted therapies for mood disorders in humans.
“Until now, little has been known about how sensitivity to regret may be altered in mood disorders like depression. For example, is regret exaggerated and do individuals hyper-ruminate on past decisions, or are those with depression numb to this emotion? Is this adaptive or maladaptive, and are individuals unable to learn from their mistakes?” says Brian Sweis, MD, PhD, an instructor in the Department of Neuroscience and resident in the Department of Psychiatry at Icahn Mount Sinai, and senior author of the study. “To date, for patients struggling with depression, there has been no clear description of regret as a defining feature of the condition.”
Building on previous work demonstrating that rats and mice are capable of processing regret-like thoughts, the Mount Sinai study pushes the boundaries of what can be captured in rodent models used for the study of mental illnesses. The authors accomplished this goal by combining sophisticated approaches in behavioral economics and chronic stress procedures with viral gene therapy to study the neural and molecular basis of complex decision making in animals.
This methodology built on principles of neuroeconomics, which is the study of how the physical limits of the brain give rise to biases we have when making decisions. This approach enabled researchers to capture how complex choices made in one’s past can impact subsequent decisions and, importantly, how the way in which individuals process or realize missed opportunities is capable of interacting with affective states when influencing future choices—the basis of regret.
The team trained mice on a decision-making task termed “Restaurant Row” during which animals navigated a maze foraging for their sole source of food (see animation). Mice were allotted a limited amount of time each day to invest in rewards of varying costs (delays randomly selected from 1 to 30 seconds signaled by the pitch of a tone) and subjective value (unique flavors tied to four separate locations, or “restaurants”). Mice chose to enter or skip each restaurant depending on the cost and flavor presented. If mice accepted an offer by entering the restaurant, they were tasked to wait out a countdown in order to earn the reward before moving on to the next restaurant. Mice displayed stable preferences of willingness to wait depending on each restaurant’s flavor. A violation in one’s own decision policy can be interpreted as the first step in constructing a situation that could invoke regret.
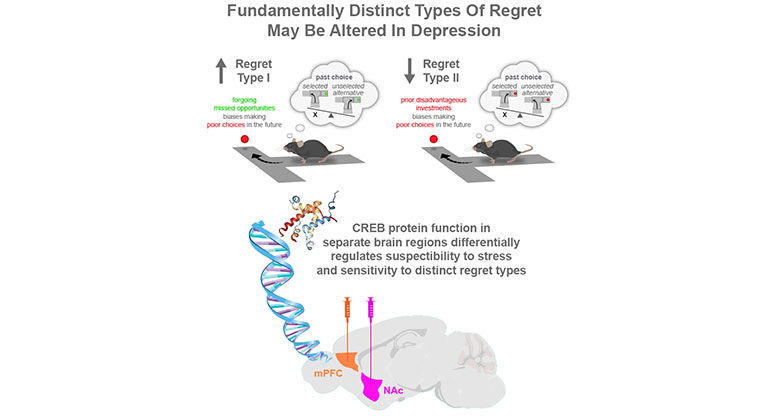
Among the major findings is the existence of two distinct types of regret that are not generic but, rather, associated with separate parts of the brain, depending on the exact nature of the missed opportunity that is being processed. Both types involve animals making mistakes. However, type one regret was defined as an “economic violation” in which animals walked away from a good opportunity only to get burned on subsequent trials (see summary figure). Conversely, type two regret was defined as decisions in which animals made poor choices to invest their limited time in offers they typically could not afford. Thus, type one regret is framed by the individual’s realization that they missed or passed up a favorable opportunity, while type two regret is characterized by facing the decision to cut one’s losses and move on. Although both types of regret may involve reflecting on the road not traveled and what could have been, type one regret emphasizes the choice of having let something good go, while type two regret emphasizes having to change one’s mind. This study found that the weight these mistakes carry in altering future decisions are biologically distinct and uniquely linked to stress-response traits.
“We discovered that stress-susceptible mice were hypersensitive to type one regret and insensitive to type two regret while, conversely, healthy mice were insensitive to type one regret and only sensitive to type two, enhanced more so in stress-resilient mice,” explains co-author Scott Russo, PhD, Professor of Neuroscience, and Psychiatry, Icahn Mount Sinai. “These findings tell us that the way the brain processes mistakes is multifactorial and linked to the ability to cope with stress, and that one type of regret is part of a healthy set of emotional traits while the other may be part of the disease process itself. Like pain, some forms of which are healthy and adaptive while others are pathological, we found that not all forms of regret are the same and they derive from different circuits in the brain.”
According to Dr. Sweis, who is currently training as a psychiatrist at Mount Sinai, the team’s research could have a significant impact on clinical practice, even by informing the way in which mental health providers interview patients with mood disorders.
“Prior to our study, professionals may not have thought to ask patients more specific questions during psychiatric evaluations detailing and subcategorizing regret with the level of delicacy we’ve outlined,” says Dr. Sweis. “Our work may improve how psychiatric interviews could be conducted to better identify what thought processes should be reinforced versus extinguished, informed by cutting-edge scientific discoveries in neuroscience and computational psychiatry. Our research could help steer clinician-patient interviews toward discerning specific circuits that may be contributing to one’s mood disorders and develop therapeutic approaches accordingly.”
The Mount Sinai researchers also discovered that a gene known to regulate many stress-sensitive responses in the brain—CREB—may independently influence the two types of regret in separate brain regions: the medial prefrontal cortex and the nucleus accumbens.
“In both humans and mice, this gene is known to promote stress resilience in the medial prefrontal cortex while conferring the opposite, vulnerability to stress, in the nucleus accumbens,” says Romain Durand-de Cuttoli, PhD, first author of the study and a postdoctoral researcher at Mount Sinai.
Until now, it remained unclear what role, if any, CREB function plays in more complex emotional processes. By experimentally manipulating CREB activity in both brain regions, the team found a biological connection and a potential molecular target to develop new therapies that could alter certain aspects of regret in a brain-region-specific manner in order to restore healthy emotional processing, while ameliorating potentially unhealthy and pathological forms of this complex emotion.
“Knowing that subtypes of regret-processing stem from different brain regions has broad implications for appreciating which brain circuits are not only driving different choices but the different ways in which we reflect on our past,” says Dr. Durand-de Cuttoli, “and how more precise interventions, whether through drug development or more invasive neuromodulation approaches, tailored to specific pathological emotional traits may be targeted to treat mood disorders more effectively.”
About the Icahn School of Medicine at Mount Sinai
The Icahn School of Medicine at Mount Sinai is internationally renowned for its outstanding research, educational, and clinical care programs. It is the sole academic partner for the eight member hospitals* of the Mount Sinai Health System, one of the largest academic health systems in the United States, providing care to a large and diverse patient population.
Ranked 14th nationwide in National Institutes of Health (NIH) funding and among the 99th percentile in research dollars per investigator according to the Association of American Medical Colleges, Icahn Mount Sinai has a talented, productive, and successful faculty. More than 3,000 full-time scientists, educators and clinicians work within and across 34 academic departments and 35 multidisciplinary institutes, a structure that facilitates tremendous collaboration and synergy. Our emphasis on translational research and therapeutics is evident in such diverse areas as genomics/big data, virology, neuroscience, cardiology, geriatrics, as well as gastrointestinal and liver diseases.
Icahn Mount Sinai offers highly competitive MD, PhD, and Master’s degree programs, with current enrollment of approximately 1,300 students. It has the largest graduate medical education program in the country, with more than 2,000 clinical residents and fellows training throughout the Health System. In addition, more than 550 postdoctoral research fellows are in training within the Health System.
A culture of innovation and discovery permeates every Icahn Mount Sinai program. Mount Sinai’s technology transfer office, one of the largest in the country, partners with faculty and trainees to pursue optimal commercialization of intellectual property to ensure that Mount Sinai discoveries and innovations translate into healthcare products and services that benefit the public.
Icahn Mount Sinai’s commitment to breakthrough science and clinical care is enhanced by academic affiliations that supplement and complement the School’s programs.
Through the Mount Sinai Innovation Partners (MSIP), the Health System facilitates the real-world application and commercialization of medical breakthroughs made at Mount Sinai. Additionally, MSIP develops research partnerships with industry leaders such as Merck & Co., AstraZeneca, Novo Nordisk, and others.
The Icahn School of Medicine at Mount Sinai is located in New York City on the border between the Upper East Side and East Harlem and classroom teaching takes place on a campus facing Central Park. Icahn Mount Sinai’s location offers many opportunities to interact with and care for diverse communities. Learning extends well beyond the borders of our physical campus, to the eight hospitals of the Mount Sinai Health System, our academic affiliates, and globally.
* Mount Sinai Health System Member Hospitals: The Mount Sinai Hospital; Mount Sinai Queens; Mount Sinai Beth Israel; Mount Sinai West (previously known as Mount Sinai Roosevelt); Mount Sinai Morningside (previously known as Mount Sinai St. Luke’s); Mount Sinai Brooklyn; New York Eye and Ear Infirmary of Mount Sinai; and Mount Sinai South Nassau (previously known as South Nassau Communities Hospital).
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.