Study Reveals a Trio of Immune Cells Vital in Response to Liver Cancer Immunotherapy
Findings may inform new approaches to cancer immunotherapy
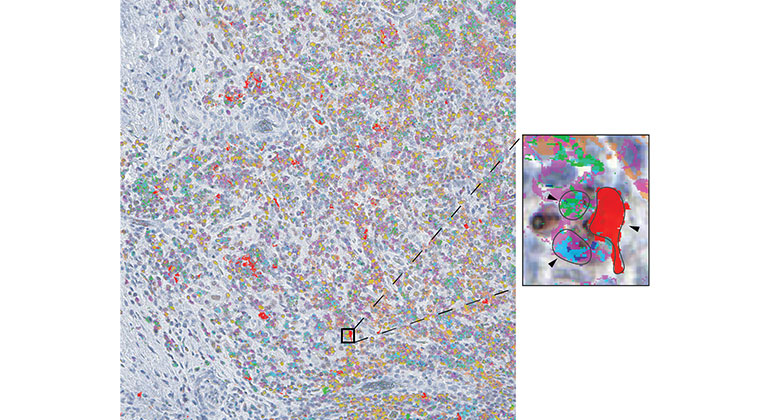
The study revealed how certain immune cell interactions in tumors facilitate response to checkpoint blockade, pointing to potential new approaches to cancer immunotherapy. Art Credit: Magen et al., Nature Medicine
Researchers at the Icahn School of Medicine at Mount Sinai have uncovered a trio of immune cells within tumor niches that are associated with immunotherapy response in hepatocellular carcinoma (HCC). HCC is the primary type of liver cancer and one of the most deadly cancers worldwide. The findings—which help explain which patients benefit from immunotherapy and which do not—were described in the June 15 issue of Nature Medicine [DOI: 10.1038/s41591-023-02345-0].
The investigators discovered that a specific niche of immune cells in tumors may be critical for reactivating exhausted T cells and enabling them to attack liver tumors upon treatment with checkpoint blockade. Also known as a PD1 inhibitor, checkpoint blockade is a type of cancer immunotherapy that can unleash the cancer-killing activity of T cells.
“While checkpoint blockade has unquestionably revolutionized cancer treatment, most patients do not respond to this immunotherapy. Understanding at the molecular level why only some patients respond will help identify novel targets for improving cancer treatment,” says senior study author Miriam Merad, MD, PhD, Director of the Marc and Jennifer Lipschultz Precision Immunology Institute and Director of the Human Immune Monitoring Center at Icahn Mount Sinai.
The researchers designed a trial that would both benefit patients and provide new data to explore why immune cells in some patients can be reactivated by immunotherapy and eradicate tumors while the same treatment fails to help other patients.
“This work follows a study our team recently published in The Lancet Gastroenterology & Hepatology reporting that immunotherapy administered before liver cancer surgery can kill tumors and likely residual cancer cells,” says Thomas Marron, MD, PhD, head of the Early Phase Trial Unit at the Mount Sinai Tisch Cancer Center, the clinical trial lead, and co-senior author of the study.
In this follow-up study, the research team analyzed tumor samples taken from 29 patients before and after treatment with checkpoint blockade. Using single-cell technology and powerful computational platforms, the team identified distinct groups of immune cells within tumors that determined which patients responded positively to immunotherapy and which did not.
These studies represent the first developments out of Icahn Mount Sinai’s TARGET platform—The Neoadjuvant Research Group to Evaluate Therapeutics, founded by Drs. Marron and Merad. TARGET’s goal is to harness the technological capabilities of the Human Immune Monitoring Center and map the molecular changes that occur in cancer and immune cells undergoing treatment to reveal precisely how immunotherapy works.
Only through understanding the mechanisms of how these revolutionary immunotherapies work in humans and the multiple mechanisms behind treatment resistance can we further improve outcomes for all patients, say the investigators.
“Reactivation of a type of T cell called CD8 T cells by checkpoint blockade was known to be critical for clearing tumor cells. Our new study shows that killer CD8 T cells are only reactivated when in close proximity to two other immune cell types: dendritic cells, which educate CD8 T cells to recognize cancer cells, and helper CD4 T cells, which aid in activating the CD8 T cells,” says Alice Kamphorst, PhD, co-senior author of the study, and Assistant Professor of Oncological Sciences at the Precision Immunology Institute.
These findings indicate that these specialized immune cell niches control the reactivation of CD8 T cells and subsequent tumor eradication by checkpoint blockade. By deciphering the molecules pivotal to the formation of these niches within tumors, the researchers intend to identify novel therapeutic targets to use in combination with PD1 blockade and test these treatment combinations via the TARGET platform.
The paper is titled “Intratumoral dendritic cell-helper T cell niches enable CD8+ T cell differentiation following PD-1 blockade in hepatocellular carcinoma.”
The remaining authors, all with Icahn Mount Sinai except where indicated, are Assaf Magen, Pauline Hamon, Nathalie Fiaschi [Regeneron Pharmaceuticals, Inc.], Brian Y. Soong, Matthew D. Park, Raphaël Mattiuz, Etienne Humblin, Leanna Troncoso, Darwin D'souza, Travis Dawson, Joel Kim, Steven Hamel, Mark Buckup, Christie Chang, Alexandra Tabachnikova, Hara Schwartz, Nausicaa Malissen, Yonit Lavin, Alessandra Soares-Schanoski, Bruno Giotti, Samarth Hegde, Giorgio Ioannou, Edgar Gonzalez-Kozlova, Clotilde Hennequin, Jessica Le Berichel, Zhen Zhao, Stephen C. Ward, Isabel Fiel, Baijun Kou, Michael Dobosz, Lianjie Li, Christina Adler, Min Ni, Yi Wei, Wei Wang, Gurinder S. Atwal, Kunal Kundu [Regeneron Pharmaceuticals, Inc.], Kamil J. Cygan [Regeneron Pharmaceuticals, Inc.], Alex Tsankov, Adeeb Rahman, Colles Price [Vizgen Inc.], Nicolas Fernandez [Vizgen Inc.], Jiang He [Vizgen Inc.], Namita T. Gupta, Seunghee Kim-Schulze, Sacha Gnjatic, Ephraim Kenigsberg, Raquel P. Deering [Regeneron Pharmaceuticals, Inc.], Myron Schwartz, Thomas U. Marron, Gavin Thurston, and Alice O. Kamphorst.
This study was funded by Regeneron Inc. In addition, the work was partially supported by National Institutes of Health grants CA224319, DK124165, CA263705, CA196521, CA257195, CA254104, CA154947, R01 AI153363, and the Mount Sinai Tisch Cancer Institute Cancer Center Support Grant P30 CA196521.
To view competing interests, please see the paper at Nature Medicine.
About the Icahn School of Medicine at Mount Sinai
The Icahn School of Medicine at Mount Sinai is internationally renowned for its outstanding research, educational, and clinical care programs. It is the sole academic partner for the eight- member hospitals* of the Mount Sinai Health System, one of the largest academic health systems in the United States, providing care to a large and diverse patient population.
Ranked 14th nationwide in National Institutes of Health (NIH) funding and among the 99th percentile in research dollars per investigator according to the Association of American Medical Colleges, Icahn Mount Sinai has a talented, productive, and successful faculty. More than 3,000 full-time scientists, educators, and clinicians work within and across 44 academic departments and 36 multidisciplinary institutes, a structure that facilitates tremendous collaboration and synergy. Our emphasis on translational research and therapeutics is evident in such diverse areas as genomics/big data, virology, neuroscience, cardiology, geriatrics, as well as gastrointestinal and liver diseases.
Icahn Mount Sinai offers highly competitive MD, PhD, and Master’s degree programs, with current enrollment of approximately 1,300 students. It has the largest graduate medical education program in the country, with more than 2,000 clinical residents and fellows training throughout the Health System. In addition, more than 550 postdoctoral research fellows are in training within the Health System.
A culture of innovation and discovery permeates every Icahn Mount Sinai program. Mount Sinai’s technology transfer office, one of the largest in the country, partners with faculty and trainees to pursue optimal commercialization of intellectual property to ensure that Mount Sinai discoveries and innovations translate into healthcare products and services that benefit the public.
Icahn Mount Sinai’s commitment to breakthrough science and clinical care is enhanced by academic affiliations that supplement and complement the School’s programs.
Through the Mount Sinai Innovation Partners (MSIP), the Health System facilitates the real-world application and commercialization of medical breakthroughs made at Mount Sinai. Additionally, MSIP develops research partnerships with industry leaders such as Merck & Co., AstraZeneca, Novo Nordisk, and others.
The Icahn School of Medicine at Mount Sinai is located in New York City on the border between the Upper East Side and East Harlem, and classroom teaching takes place on a campus facing Central Park. Icahn Mount Sinai’s location offers many opportunities to interact with and care for diverse communities. Learning extends well beyond the borders of our physical campus, to the eight hospitals of the Mount Sinai Health System, our academic affiliates, and globally.
-------------------------------------------------------
* Mount Sinai Health System member hospitals: The Mount Sinai Hospital; Mount Sinai Beth Israel; Mount Sinai Brooklyn; Mount Sinai Morningside; Mount Sinai Queens; Mount Sinai South Nassau; Mount Sinai West; and New York Eye and Ear Infirmary of Mount Sinai.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, employing 48,000 people across its hospitals and more than 400 outpatient practices, as well as more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.