Where You Live Matters: A First-of-Its-Kind Study Illustrates How Racism Is Interrelated With Poor Health
Study published in JAMA Network Open points to discrete factors, like voting participation, employment, education, and housing, that may serve as promising targets for interventions
A team of health equity researchers from several institutions has leveraged a complex web of data to test a hypothesis: That structural racism is associated with resources and structures at the neighborhood level that are closely associated with poor health. What they found in an analysis of highly localized, community level data illustrates how racism is deeply interrelated with poor health outcomes.
Dinushika Mohottige, MD, MPH, Assistant Professor of Population Science and Policy, and Medicine (Nephrology), at the Icahn School of Medicine at Mount Sinai, served as first author of a paper published today in the journal JAMA Network Open that details the study.
Dr. Mohottige and her senior author and long-time mentor, L. Ebony Boulware, MD, MPH, Dean of Wake Forest University School of Medicine, describe in detail how neighborhood prevalence of chronic kidney disease (CKD), diabetes, and hypertension are strongly associated with an increased burden of structural racism indicators.
The research team conducted an observational cross-sectional study in Durham County, North Carolina, using public data sources and deidentified electronic health records to explore how a comprehensive collection of data points associate the presence of structural racism and the neighborhood prevalence of these three chronic health conditions.
“It was important to look at these three conditions because they are interconnected and highly associated with heart disease, as well as quality and length of life. Importantly, Black people share a disproportionate burden of these three illnesses,” said Dr. Mohottige, a member of Icahn Mount Sinai’s Institute for Health Equity Research who specializes in kidney health equity and formerly practiced at Duke University with Dr. Boulware. They collaborated with colleagues from Duke, the University of North Carolina at Chapel Hill, North Carolina State University, and the Feinstein Institutes for Medical Research.
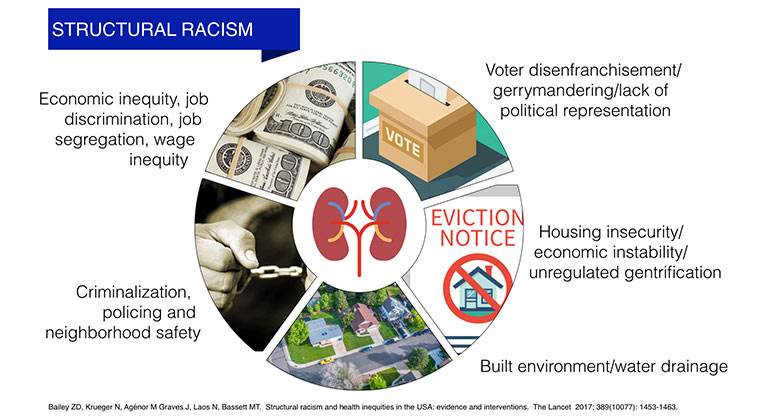
The authors explain that structural racism is defined as how societies foster discrimination through a series of systems that are reinforcing, such as housing, education, and unemployment. “These systems cascade into discriminatory beliefs, values, and the distribution of resources,” says Dr. Boulware.
“Dr. Mohottige and I agreed it was important to tap the unusual data assets available in Durham to learn how we can improve the health of communities and individuals by identifying the factors that may affect their health the most. Our goal was to use the data to help us identify possible interventions,” says Dr. Boulware. “Data which measure health outcomes such as kidney disease and diabetes––and which also measure social determinants of health, including information on the built environment and reported neighborhood violence––help us understand how the conditions where people live affect their well-being. This is especially true for groups that, because of their race or ethnicity, historically experience worse health outcomes when compared to others.”
The result of their work, incorporating thousands of data points related to where people live at the most localized level, says Dr. Boulware, is a first-of-its-kind observational study of associations of structural racism constructs with the health of individuals residing in these neighborhoods. “This study fills an important evidence gap and helps us identify factors which might be targeted to address community health inequities,” says Dr. Mohottige.
The researchers studied data of aggregate estimates of prevalence of chronic conditions for each of 150 residential neighborhoods in Durham using the Durham Neighborhood Compass, a unique data asset created by public health officials; a corresponding website, Durham Community Health Indicators Project, provides a user-friendly interface in lay language.
Along with the uniquely detailed and comprehensive Compass data, the researchers pulled data from two main buckets. Through global/composite indicators such as the area deprivation index, they gleaned data revealing the extent of Durham’s stark neighborhood advantage and disadvantage. The discrete indicators they drew upon revealed downstream factors widely thought to represent sociopolitical manifestations of structural racism, including reported crime, evictions, police shootings, and election participation. “Very limited evidence exists to tie together these structural racism constructs with the aggregate health of individuals in a given neighborhood using electronic health data and rigorous assessments of chronic conditions,” says Dr. Mohottige.
The team found that:
- Residential neighborhoods with the highest prevalence of CKD, diabetes, and hypertension, tended to be in neighborhoods with the lowest proportions of White residents, and vice versa.
- Neighborhoods with the highest prevalence of CKD, diabetes, and hypertension tended to be in areas with the lowest income and higher area deprivation. They also had the lowest rates of college education.
- A greater burden of most discrete indicators of structural racism (examples include reported violent crime, eviction rates, election participation, income, and poverty) was associated with greater neighborhood prevalence of the three diseases.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.