Women With Atrial Fibrillation Significantly Benefit From Pulsed Field Ablation Procedures
Mount Sinai-led study is the first to show there are no sex disparities in patient outcomes with this new technology
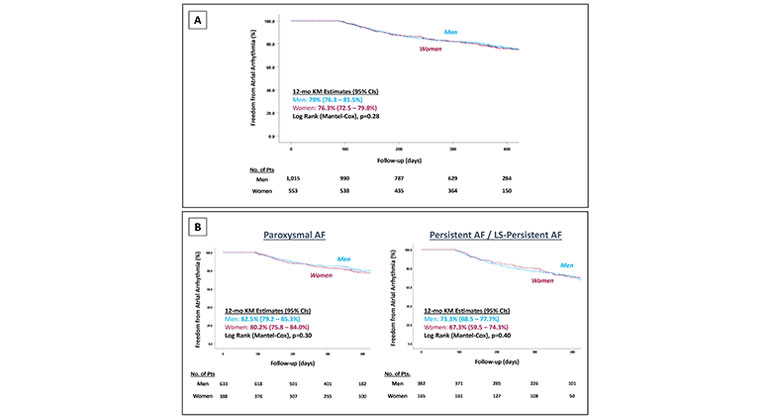
Description: The primary effectiveness outcomes are shown for both the full patient cohort (A) and separated by atrial fibrillation (AF) subtype: paroxysmal AF (B) vs persistent AF/long-standing (LS)–persistent AF (C)
Women with atrial fibrillation (AF) undergoing a procedure called pulsed field ablation (PFA) have just as good outcomes as men with AF undergoing the same procedure, according to a large-scale international study led by the Icahn School of Medicine at Mount Sinai.
This study is the first to compare sex outcomes for AF patients undergoing PFA, which is a new technology and the latest ablation modality that can be used to restore a regular heartbeat. The results also show PFA is safe and just as effective for men as for women. Findings were published October 5 in JAMA Cardiology.
“These results are important, as women are underrepresented in prior ablation studies and the results have been mixed with regards to both safety and effectiveness using conventional ablation strategies such as radiofrequency or cryoablation,” says first author Mohit Turagam, MD, Associate Professor of Medicine (Cardiology) at Icahn Mount Sinai.
AF is an irregular heartbeat or heart rhythm disorder; 2.7 million Americans live with some form of it. Patients with AF can undergo a catheter procedure to treat this abnormal heart rhythm, called catheter ablation. This procedure involves making scars in small areas in the heart involved in the abnormal rhythm, which prevents abnormal electrical signals or rhythms from moving through the heart.
Two types of ablation are currently in common use: radiofrequency ablation, which uses heat energy to eliminate the problem area, and cryoablation, which uses cold energy. These ablation modalities are associated with increased risk of potential complications, including damage to the esophagus, pulmonary vein stenosis, and phrenic nerve injury. PFA is a new type of ablation that does not use temperature, but instead short, high-energy electrical pulses that target mainly cardiac cells. This catheter procedure is more precise than radiofrequency and cryoablation, and does not cause damage to the esophagus, pulmonary veins, or phrenic nerve (which controls the diaphragm and is essential for breathing).
The researchers did a retrospective analysis of 1,568 patients from the Multi-National Survey on the Methods, Efficacy, and Safety on the Post-Approval Clinical Use of Pulsed Field Ablation (MANIFEST-PF). This is a large multinational registry from 24 European centers and includes patients who underwent their first-ever PFA for AF between March 2021 and May 2022 (after the device received regulatory approval in Europe). The researchers categorized patients by sex and evaluated clinical outcomes of PFA within these groups. They studied the elimination of AF, and adverse events such as esophageal complications, pulmonary vein stenosis, phrenic nerve injury, pericardial tamponade (fluid accumulation in the heart), and vascular injury.
The results showed no significant difference in recurring atrial arrhythmia in men versus women. Specifically, 79 percent of men versus 76 percent of women did not have recurring atrial arrhythmia after PFA, a difference that was not statically significant. The rate of patients needing a second ablation were similar between sexes, with men at 8.3 percent versus women at 10 percent, also not statically significant. Among the patients who underwent a second AF ablation, pulmonary vein isolation durability was significantly higher in women than in men (63 percent versus 37.8 percent), meaning they were less likely to have an additional ablation in their pulmonary veins. Complication rates from the procedure were low overall, and did not differ significantly by sex (women at 2.5 percent versus men at 1.5 percent).
“For the last few years, the emerging data with pulsed field energy has been quite promising for the treatment of atrial fibrillation. This current analysis of the large-scale MANIFEST-PF registry demonstrates that the benefits are not just limited to men; women derive the same level of success at one year, 76.3 percent, with a low complication rate of 2.5 percent. Thus, women should not be denied the beneficial, life-enhancing procedure of catheter ablation for atrial fibrillation,” says senior author Vivek Reddy, MD, The Leona M. and Harry B. Helmsley Charitable Trust Professor of Medicine in Cardiac Electrophysiology at Icahn Mount Sinai.
**Dr. Reddy is a paid consultant of Boston Scientific Corporation. He has not been compensated in connection with this press release.
Figure: Kaplan-Meier (KM) Analysis of Freedom From Atrial Arrhythmia by Sex
A – Full Patient Cohort
B – Paroxysmal AF
C – Persistent AF/LS-persistent AF
Mount Sinai Fuster Heart Hospital is one of the world’s top four hospitals in Cardiology/Heart Surgery
Mount Sinai Fuster Heart Hospital ranks No. 1 in New York and No. 4 globally according to Newsweek’s “The World’s Best Specialized Hospitals.” The Mount Sinai Hospital is also No. 1 in New York for cardiology, cardiac surgery, and vascular surgery, according to U.S. News & World Report®.
It is part of Mount Sinai Health System, which is New York City's largest academic medical system, encompassing eight hospitals, a leading medical school, and a vast network of ambulatory practices throughout the greater New York region. We advance medicine and health through unrivaled education and translational research and discovery to deliver care that is the safest, highest-quality, most accessible and equitable, and the best value of any health system in the nation. The Health System includes approximately 7,400 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report's® “Best Hospitals” Honor Roll for 2023-2024.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.