Mount Sinai Researchers the First to Apply Single-Cell Analysis to Reveal Mechanisms of a Common Complication of Crohn’s Disease
Study identifies key pathways underlying perianal fistula, a complication that is more prevalent and severe in African American populations
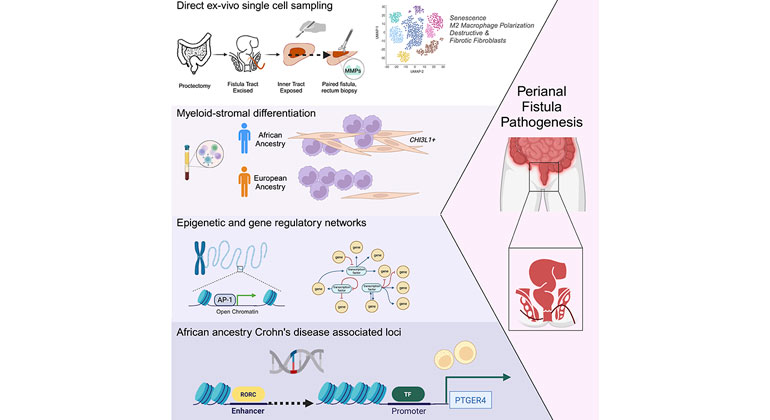
Photo credit: Courtesy of Med/Cell Press (Elsevier)
Multimodal analyses of cells from abnormal tunnels in Crohn's disease converge to illuminate underlying
Mount Sinai researchers have published the first study to use single-cell analysis in identifying several pathophysiological mechanisms of abnormal passageways in the digestive system known as perianal fistulae, a common complication of Crohn’s disease. These findings were published in the journal Med on April 24.
Crohn’s disease is an inflammatory bowel disease that causes chronic inflammation at any part of the gastrointestinal (GI) tract and impacts more than half a million people in the United States. Perianal fistulae, abnormal connections between the anal canal and perianal skin, are a common complication of Crohn’s disease that often result in painful abscesses and impact patients’ quality of life.
This Mount Sinai study is the first to apply single-cell transcriptomics of perianal fistulous tracts, and to recruit Black patients with the chronic condition for a diverse and comprehensive study cohort. Patients with African ancestry have been substantially underrepresented in genome-wide association studies of Crohn’s disease, and inflammatory bowel disease overall, reflecting in part the lower prevalence of Crohn’s disease in African American populations compared to patients with European ancestry. However, patients of African ancestry are about twice as likely to have perianal fistulae, according to studies in adult and pediatric populations.
The researchers profiled more than 140,000 single cells from diverse Crohn’s disease patients with perianal fistulae. The team identified several key pathways underlying fistulizing Crohn’s disease, including cellular aging and loss of proliferation, reaction to microenvironmental stimuli, and a destructive gene signature in connective tissues that is unique to perianal fistulae. The researchers also determined that subpopulations of fibroblasts—cells forming the connective tissues—with this destructive gene signature may originate from mononuclear cells in the immune system, a phenomenon observed in greater magnitude from patients with African ancestry. The experts found evidence for key transcription factor binding events in relevant gene promoter regions that suggests a potential epigenetic phenomenon underlying this apparent difference in cell behavior between patients of African and European ancestry.
“Circulating blood monocytes can traffic to disease tissues and form a critical first step in fighting microbes throughout the body,” said corresponding author Judy H. Cho, MD, Dean and Ward-Coleman Chair in Translational Genetics at the Icahn School of Medicine at Mount Sinai. “In this study, we have defined population-specific differences in how blood monocytes respond, which contribute to the higher rates of perianal fistulous complications in African American patients with Crohn’s disease.”
A range of anti-inflammatory medications can treat Crohn’s disease, but they show limited efficacy for closure of perianal fistula tracts. In severe cases, patients may require surgical removal of all or part of the rectum. But researchers said their findings provide avenues to identify new therapeutic options. The team said future studies should examine similar epigenetic patterns in white blood cells of the immune system from diverse, healthy patients and from patients with other immune-mediated inflammatory diseases to further explore the role of the transcription factor underlying race or ancestry-based disparities.
“We have leveraged transcriptomic, epigenetic, genetic, cellular, and tissue-based data from patients with a history of this devastating complication to better understand reasons for the discrepancy in prevalence between Black and white patients,” said first author Rachel M. Levantovsky, PhD, who is working on her MD in the Mount Sinai Medical Scientist Training Program. “Our discovery of unique fistula fibroblasts, distinct monocyte differentiation in African-ancestry individuals, and key transcription factor binding events helps us illuminate mechanistic underpinnings of perianal fistula—critical for the optimization of future treatment.”
The study was supported by funding from the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (U01DK062422, U24DK062429, R01DK123758, and F30DK127736), Leona M. and Harry B. Helmsley Charitable Trust, Sanford J. Grossman Charitable Trust, and David and Margot Lowy Foundation Trust.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
Researchers Identify Opportunities to Advance Genomic Medicine
Jan 27, 2020 View All Press ReleasesDrug Resistance Signature Discovered in Crohn’s Disease
Aug 29, 2019 View All Press Releases