- New York, NY
- (January 22, 2025)
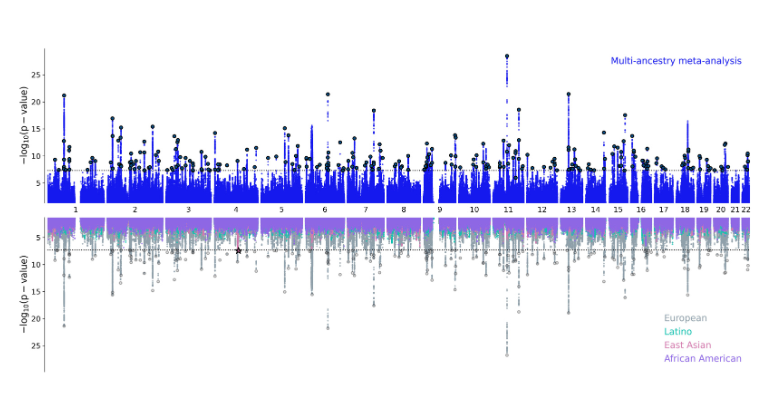
In the largest genome-wide study of bipolar disorder to date, an international team of psychiatric genetics researchers has identified 298 regions of the genome containing DNA variations that increase risk for the disorder—a more than four-fold increase over the number previously identified, according to research published in Nature [https://doi.org/10.1038/s41586-024-08468-9] on Wednesday, January 22.
The study—the first large multi-ancestry genomic analysis of the disorder to include data from people of European, East Asian, African American, and Latino ancestries—also identifies a new region associated with an increased risk for the disorder within the East Asian samples. Cross-referencing a range of methods, including fine-mapping and other variant-to-gene-mapping approaches, the team identified 36 genes suspected to be relevant to bipolar disorder.
Bipolar disorder is an often lifelong mood disorder that impairs quality of life and functional ability, and is associated with suicidality. It affects an estimated 40-50 million people worldwide. Bipolar disorder is clinically heterogeneous, encompassing distinct subtypes 1 and 2. Bipolar disorder type 1 is characterized by episodes of both mania and depression, while bipolar disorder type 2 includes episodes of hypomania (a less severe form of mania) and depression. Despite the prevalence of bipolar disorder, it can take an average of eight years to get a proper diagnosis, and much remains unknown about the biology of the condition.
To help elucidate bipolar disorder’s underlying biology, an international team of scientists from within the Psychiatric Genomics Consortium conducted a genome-wide association study, scanning the DNA of 2.9 million study participants from cohorts worldwide to identify genetic markers that were more common in those with the condition. This involved scanning more than 6.7 million common variations in the DNA sequences among the study participants, more than 158,000 of whom experience bipolar disorder.
“It is well established that bipolar disorder has a substantial genetic basis, so identifying DNA variations that increase risk is of paramount importance to understanding the condition’s genetic architecture. In addition to identifying 298 regions of the genome that contain variations that increase risk for bipolar disorder, the 36 key genes we identified as being linked to the condition can now be followed up in a range of experiments to uncover the biological mechanisms through which each relates to the disorder,” says Niamh Mullins, PhD, Assistant Professor in the Departments of Psychiatry, and Genetics and Genomic Sciences, and the Charles Bronfman Institute for Personalized Medicine at the Icahn School of Medicine at Mount Sinai and one of the senior authors of the paper. “The newly identified genes may also be used in experiments to explore new drug targets and drug development for bipolar disorder.”
The study team also found differences in the genetic characteristics of bipolar disorder between clinical (patients recruited from hospital inpatient or outpatient units), community-based (participants in general population biobanks), and self-reporting (participants in online personal health surveys) participants. These genetic differences are likely to be driven by a higher prevalence of bipolar subtype 1 in the clinical samples versus a higher prevalence of bipolar subtype 2 in the self-reporting samples, which highlights the need for researchers to be mindful of the data-gathering strategies used within their studies of the condition.
According to the research team, the genetic signal of bipolar disorder is related to specific brain cell types, including GABAergic interneurons and medium spiny neurons, in the prefrontal cortex and hippocampus. They also found that cells in the intestine and pancreas are involved, although more research is necessary to further understand this biology.
“Although this work does not immediately impact patient care, it opens the possibilities for long-term positive impact for patients and their families who are impacted by this widespread disorder,” said Ole Andreassen, MD, PhD, Professor of Psychiatry at the Institute of Clinical Medicine and Oslo University Hospital, and senior author of the paper. “Our research paves the way for the development of improved treatments, earlier interventions, and precision medicine approaches that will support clinicians in their decision-making to enable them to manage the condition in the most effective way for each patient.”
The Psychiatric Genomics Consortium (PGC) is an international consortium of scientists dedicated to studying the genetic basis of psychiatric disorders and includes more than 1,700 researchers from over 65 countries.
”This research would not have been possible without the collaborative efforts of scientists worldwide that enabled the study of hundreds of thousands of DNA sequences,” said Kevin O’Connell, PhD, researcher at the University of Oslo and first author of the paper.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, employing 48,000 people across its hospitals and more than 400 outpatient practices, as well as more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.