Mount Sinai Researchers Uncover Barriers to Opioid Accessibility for Seriously Ill Patients
In a study published in NEJM Catalyst Innovations In Care Delivery, researchers at the Icahn School of Medicine at Mount Sinai describe how measures to curb opioid overdoses in the general population have compromised a critical cornerstone of palliative care. Opioids are medically necessary analgesics for the relief of moderate to severe pain in patients with cancer and other serious illnesses, such as acute sickle cell crises, and for patients following surgery.
“The opioid crisis of overdose deaths remains omnipresent; however, a new threat has emerged among vulnerable populations who need these medicines as first-line treatment for their pain, which can be severe,” says lead author Rebecca Rodin, MD, Assistant Professor of Geriatrics and Palliative Medicine, Icahn Mount School of Medicine at Mount Sinai, who specializes in palliative medicine. “We hope our findings will lay the foundation for deeper dialogue to restore balance between opioid excess and access.”
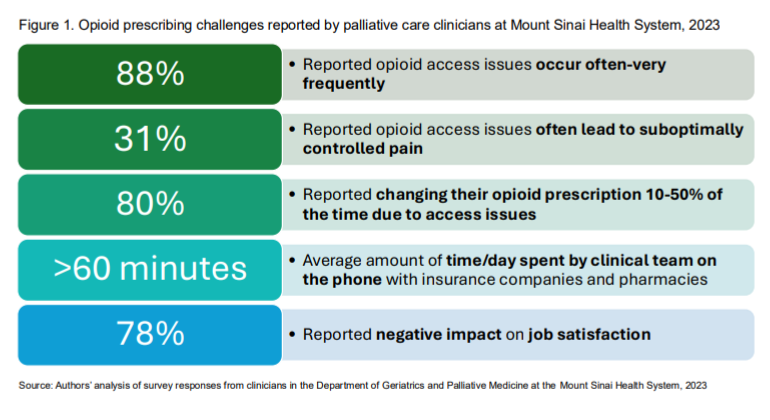
In their paper, the authors share several important findings gleaned from a 2023 needs assessment survey of clinicians within Mount Sinai’s Brookdale Department of Geriatrics and Palliative Medicine. While the survey was limited to 52 clinicians, it unearthed significant hurdles in three domains: pharmacy-related issues, such as low medication supplies; insurance-related obstacles to prescribing, including preauthorization requirements and pill limits; and communication issues, such as long hold times when physicians attempted to call pharmacists:
- 88 percent reported opioid access issues occurring often.
- 80 percent said they changed their opioid prescribing up to 50 percent of the time due to limited availability of the needed medications.
- 31 percent said access issues often led to suboptimal pain control.
- Clinical teams said they spent more than one hour every day on the phone with insurance companies and pharmacies.
Of critical concern, say the authors, is scattered and uneven availability among pharmacies.
“Our clinicians told us that in New York City’s outer boroughs, such as the Bronx, Brooklyn, and Queens, they encountered much greater difficulty obtaining opioids where we treat higher concentrations of underrepresented patients who are socioeconomically vulnerable,” says Dr. Rodin. To improve access issues, Dr. Rodin and colleagues developed a series of targeted quality improvement initiatives at two inpatient hospitals and three outpatient clinics across the Mount Sinai Health System. These initiatives are:
Collaboration and Mutual Learning With Pharmacy Leaders
This initiative leveraged engagement with Mount Sinai pharmacy leaders to optimize supply quotas and ensure that frequently prescribed opioids were in stock. This effort aimed to educate pharmacies about the underlying rationale and necessity for these analgesics. The team also learned from the pharmacies about impediments, including concerns in neighborhoods with high crime, robbery, and theft; fears about Drug Enforcement Administration crackdowns and potential liability; and concerns about reimbursement for costly medicines not fully reimbursed by insurance.
Continuing Education Series
The researchers developed tailored education series and distributed guides to providers in internal medicine and oncology who most often admit and discharge seriously ill patients, in addition to palliative care providers who commonly prescribe opioids for their patients. Key topics included reviews of common formulations and doses for pain; guidance on writing prescriptions; anticipating and handling prior authorizations; processes for communicating between clinicians and pharmacies prior to discharge; and ways to improve communication around discharge orders for opioids.
"Our study underlines critical access challenges that impact our palliative care patients in the community, but also the need to address the very important requirement for opioids at the point of hospital discharge to ensure continued symptom management. Improving clinician knowledge and empowering discharging teams to effectively navigate outpatient opioid prescribing is imperative to ensure smooth care transitions,” says senior author Joanna Chen, MD, MPH, Assistant Professor of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, who specializes in palliative care.
Dissemination of Guide Identifying Preferred Pharmacies
Knowing which pharmacies will have medicines in stock presents a critical time-saver for doctors, says Dr. Rodin. Her team developed a guide to preferred pharmacies, updated in real time through collaboration, with practical suggestions on how to complete prior authorizations.
“Our strategies have been effective within the Mount Sinai ecosystem, but they do not address root causes of barriers which can include a number of factors, such as much broader supply chain shortages at the regional and national level, public and private coverage policies, and pharmacy stocking and dispensing practices. We need to do more to address these barriers,” said Dr. Rodin. She and her co-authors recommend refinements in medical education, research into barriers and clinical guidelines, and policy.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, employing 48,000 people across its hospitals and more than 400 outpatient practices, as well as more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.