
The Milton and Carroll Petrie Department of Urology
Our renowned team of physician-scientists is addressing a variety of challenges, including those presented by bladder, kidney, and prostate cancers.
The Milton and Carroll Petrie Department of Urology
At the Milton and Carroll Petrie Department of Urology at the Icahn School of Medicine at Mount Sinai, our renowned team of physician-scientists is addressing a variety of challenges, including those presented by bladder, kidney, and prostate cancers.
This report highlights:
- Our 2nd International Prostate Cancer Symposium and Inaugural World Congress of Urologic Oncology at The Mount Sinai Hospital
- A case involving renal cell carcinoma and a ren arcuatus that demonstrates how doctors at Mount Sinai are able to manage complex cases with low complication rates, minimal impact, and quick patient recovery
- Two major research initiatives designed to combine clinical and behavioral research in keeping with our holistic approach to helping prostate and bladder cancer patients manage their treatment
- Treating a patient with a history of urological complications and chronic conditions to ensure the best possible outcome for recovery and long-term health
- Combining expertise in robotic surgery and clinical trials with a novel surgical approach that demonstrates how innovation in treatment can accomplish a successful result in a patient with advanced bladder cancer
International Symposium Features Renowned Faculty Experts and Complex Live Surgeries
More than 80 invited faculty provided expert and thought-provoking presentations and debates at the 2nd International Prostate Cancer Symposium and Inaugural World Congress of Urologic Oncology at The Mount Sinai Hospital. The symposium also featured challenging case studies and live Mount Sinai–led surgical demonstrations showcasing advanced techniques for prostate and kidney surgery.
Hosted by the Milton and Carroll Petrie Department of Urology at the Icahn School of Medicine at Mount Sinai, the September 2017 symposium was held in collaboration with the Society of Urologic Robotic Surgeons and the Endourological Society. More than 500 medical professionals, physicians, and nurses attended the three-day event, which included more than 100 presentations delivered by world-renowned experts in the fields of bladder, kidney, and prostate cancer.
“It was an honor for us to welcome so many leaders to this event,” says Ash Tewari, MBBS, MCh, the Kyung Hyun Kim, MD Chair in Urology at the Mount Sinai Health System and director of the symposium. “It was a rare occasion to come together with our colleagues to celebrate accomplishments, survey emerging technologies and expertise, and look at how we can continue to be innovative in the care we provide patients.”

The event opened with the Hans E. Schapira Lecture, named for the late Mount Sinai physician whose research greatly advanced the understanding and treatment of urologic disease. Patrick Walsh, MD, the University Distinguished Service Professor of Urology at the
James Buchanan Brady Urologic Institute at Johns Hopkins School of Medicine, delivered the lecture “How Nerve Sparing Changed the Outcome of Prostate Cancer.” He discussed the evolution of this technique, particularly the introduction of robotic surgery, and offered a future vision for improved success in restoring potency and continence after surgery.
Among the primary highlights of the symposium were the live 3D robotic procedures broadcast to the audience from the operating room. The surgeries were performed by Dr. Tewari and Ketan Badani, MD, Vice Chair of Urology and Robotic Operations at the
Mount Sinai Health System and Director of the Comprehensive Kidney Cancer Program. Each surgery was selected to showcase advanced techniques and expertise for restoring potency and continence and for ensuring negative margins when performing prostate and kidney surgeries, which have made Mount Sinai one of the busiest robotic surgical programs in the United States for bladder, kidney, and prostate cancer.
In one surgery, Dr. Tewari demonstrated his use of the NeuroSAFE procedure for da Vinci robot-assisted radical prostatectomy to ensure negative margins. In a second surgery, he highlighted reconstruction techniques for restoring urinary continence. Dr. Badani performed a challenging robotic partial nephrectomy involving an obese patient who had a 5 cm lesion, fibrotic fat surrounding the kidney, and considerable scarring from previous surgeries. Demonstrating his FAST (First Assistant Sparing Technique) approach, Dr. Badani removed the lesion with merely 11 minutes of warm ischemia time. The patient was discharged the next day and remains tumor free.
Each surgery was transmitted in real time, with 4K resolution (or ultra-high definition, the standard for movies), giving all participants the same view as the operating surgeon, and a panel of experts provided commentary during the procedure, addressing questions from the audience regarding particular techniques.
"Most of the symposium participants are familiar with robotic surgery. But with these live surgeries we were able to teach them advanced techniques in areas such as restoration of continence and potency that they can use to provide enhanced care to their patients," Dr. Tewari says.
Other keynote presenters included:
- Inderbir S. Gill, MD, Chair and Distinguished Professor of Urology at the Keck School of Medicine of the University of Southern California, who delivered the lecture “The Changing Face of Urologic Oncologic Surgery Over 15 Years: The Impact of Robotics.” He discussed how robotic surgery has improved outcomes for patients with urologic cancers. Dr. Gill also presented a meta-analysis of data that demonstrated the advantages of robotic surgery versus open and laparoscopic approaches to bladder, kidney, and prostate cancer.
- Robert Uzzo, MD, Chair of the Department of Surgical Oncology at Fox Chase Cancer Center of the Temple University Health System, presented the lecture “Adjuvant Therapy in Renal Cell Carcinoma—Where Are We in 2017?” He reviewed current research and development initiatives and offered insights on their potential to advance patient treatment.
- Peter Wiklund, MD, PhD, Professor of Urology and Chairman of the Department of Molecular Medicine and Surgery, Section of Urology, at the Karolinska Institutet in Sweden, and Khurshid Guru, MD, Chair of the Department of Urology and Director of Robotic Surgery at Roswell Park Cancer Institute, presented the lecture “ERAS Protocol,” an overview of the enhanced recovery pathway for bladder cancer patients, and provided examples of how it is improving patient outcomes.
These presentations informed several formal debates among leading experts on topics that included the best methods for treating high-risk cancer, the merits of creating urinary diversions using robotic versus open surgery, and whether biopsies should be performed in cases involving kidney tumors.
The symposium also offered an opportunity to celebrate a legacy of advancements in urologic research and treatments. At a session marking the 75th anniversary of the Department of Urology at Mount Sinai, faculty members from the Icahn School of Medicine and two former Department chairs led attendees through a series of presentations on the history of the clinical program and the recent expansion of the Department with the creation of the Mount Sinai Health System.
"We wanted to celebrate Mount Sinai’s legacy of innovation and contributions to the field, particularly in understanding cancer genomics and biology," Dr. Badani says. “By looking back, we are able to provide context for where we want to go and how we will continually research and implement new technologies, drug therapies, and treatments.”
Abstracts from the presentations have been published in the Journal of Endourology, and the Society of Urologic Oncology has committed to producing a series of seminar-related issues for its peer-reviewed journal. Planning has begun for next year’s symposium, scheduled for September 6 to 9, 2018, and organizers hope it will open doors for more research partnerships.
“Participants have an opportunity to learn more about the work that is going on in this field and look for opportunities to collaborate in the research and development of new approaches to treatment,” Dr. Badani says.
Leaders from The Tisch Cancer Institute at the Icahn School of Medicine and the Lillian and Henry M. Stratton-Hans Popper Department of Pathology and Laboratory Medicine at the Mount Sinai Health System served as associate directors of the symposium. They included: Nina Bhardwaj, MD, PhD, Professor of Medicine (Hematology and Medical Oncology); Carlos Cordon-Cardo, MD, PhD, the Irene Heinz Given and John LaPorte Given Professor and Chair of the Department of Pathology at the Mount Sinai Health System; and William Oh, MD, Chief of the Division of Hematology and Medical Oncology, Professor of Medicine, and Urology, the Ezra M. Greenspan, MD Professor in Clinical Cancer Therapeutics, and Associate Director for Clinical Research at The Tisch Cancer Institute.
“This event was an academic and administrative success because of the participants, the speakers and faculty, our award recipients, and the team at Mount Sinai who put this together. I look forward to a similar event next year,” Dr. Tewari says.
Complex Robotic Partial Nephrectomy: Endophytic Tumor in the Isthmus of a Horseshoe Kidney
A recent case involving renal cell carcinoma and a ren arcuatus, or horseshoe kidney, demonstrates how doctors at Mount Sinai are able to manage complex cases with low complication rates, minimal impact, and quick patient recovery.

Ketan K. Badani, MD, Vice Chair of Urology and Robotic Operations and Director of the Comprehensive Kidney Cancer Program at Mount Sinai Health System, saw a 64-year-old patient who had been diagnosed with a kidney tumor by her primary care physician. Before seeing Dr. Badani, who is also a Professor of Urology at the Icahn School of Medicine at Mount Sinai, the patient had consulted with several doctors who proposed open surgery due to the complex tumor location on the isthmus of the horseshoe kidney. This can result in a very high risk of bleeding and other complications from surgery. The patient was looking for a novel, minimally invasive approach to resecting the tumor.
Given the extremely variable and unique vascular anatomy of a horseshoe kidney, Dr. Badani ordered a high-resolution 3D rendering CT scan to gain a better understanding of the patient’s anatomy. The CT scan revealed that the tumor was completely endophytic in the isthmus of the kidney, only millimeters away from the aorta. The tumor could not be seen protruding from the kidney; therefore, ultrasound would be required to locate the tumor so that it could be resected.
As a result of the patient’s unique anatomy, several arterial branches supplied the region of the tumor behind the kidney, arising directly from the aorta, which could not be controlled during a partial nephrectomy.

Dr. Badani concluded that the best course of treatment for the patient would be a robotic partial nephrectomy using a technique he developed, called FAST (First Assistant Sparing Technique), to reduce ischemia time during the resection. Since the blood supply to the isthmus of the kidney could not be controlled, this would happen “off-clamp,” so the area would continue to have active blood flow during the resection. Every minute would count.
Dr. Badani performed the robotic partial nephrectomy assisted by his highly experienced surgical team. The operation took approximately two hours and was performed through five keyhole incisions. After clamping the main renal artery, Dr. Badani injected indocyanine green, which confirmed that the isthmus was still perfused directly from the aortic branches. Using real-time ultrasound to locate the tumor, Dr. Badani resected it using the FAST approach, removing the lesion and reconstructing the defect in only 12 minutes. The total blood loss was less than 100 ml, and the patient was discharged after an overnight stay.
The 4 cm tumor was completely resected with clear margins, and the final pathology showed that it was a renal cell carcinoma. The patient will be monitored with annual CT scans, but Dr. Badani considers the patient cured.
"This case represents an example of extremely challenging anatomy along with a difficult tumor location,” Dr. Badani says. “Given our breadth of experience with robotic kidney surgery, even this difficult scenario can be accomplished as a routine partial nephrectomy. These are the kinds of very complex cases we see every day, and our robotic approach allows us consistently to achieve positive outcomes for our patients."

The Department of Urology’s kidney cancer program continues to innovate and push research breakthroughs that will improve patient care, and the patient was enrolled in two clinical trials in which Dr. Badani is the primary investigator.
One trial is a randomized study being conducted at The Mount Sinai Hospital that is exploring the potential to regenerate normal kidney tissue following robotic surgery using amniotic stem cells. “Preserving kidney function after cancer surgery will decrease the risk of dialysis in the future, leading to a dramatic effect on both quality of life and overall survival for patients,” Dr. Badani says.
The second trial is a genomic and biomarker discovery study. Dr. Badani is working with the Department of Urology’s basic science team to create one of the largest biobanks for kidney cancer that will allow researchers to examine tumor cells, blood, and urine samples for gene sequences and protein markers that they hope will lead to the first screening test for kidney cancer. “I am very proud of our research team. We are embarking on important work that can transform kidney cancer diagnosis, treatment, and survival,” Dr. Badani says.
Research About Patients on Active Surveillance and Undergoing Stoma Surgery
The Department of Urology at the Icahn School of Medicine at Mount Sinai is conducting two major research initiatives under the direction of Nihal Mohamed, PhD, Director of Behavioral Research, designed to combine clinical and behavioral research in keeping with the Department’s holistic approach to helping prostate and bladder cancer patients manage their treatment.

Active Surveillance for Prostate Cancer Patients
Active surveillance is a viable option for some low-risk prostate cancer patients. But these patients need more information than they typically receive to make informed decisions.
Behavioral Research, designed to combine clinical and behavioral research in keeping with the Department’s holistic approach to helping prostate and bladder cancer patients manage their treatment.
According to preliminary data on active surveillance from Dr. Mohamed’s research at the Icahn School of Medicine, a number of factors influence a patient’s decision to choose this option.
The data come from 28 low-risk prostate cancer patients on active surveillance, with an average age of 65, and involved in-person interviews and focus groups. The data indicate that the key factors contributing to a patient’s decision to choose active surveillance were: trust in the physician, the treatment information provided by the care team, participation of a spouse in the decision making, and a desire to avoid sexual and urinary side effects. More than one-third of the patients reported having unmet informational needs before making a final decision.
In a related but separate study, Dr. Mohamed is examining racial and cultural disparities in active-surveillance treatment among African American and Hispanic men. She plans to study 400 men through focus groups and surveys.
The U.S. Department of Defense, as part of its Prostate Cancer Research Program, is supporting the research on active surveillance.
Improved Education for Bladder and Colorectal Cancer Patients Undergoing Stoma Surgery
Early promotion of stoma care skills is critical to help patients after ostomy. However, the needs of these patients are often neglected. Dr. Mohamed’s studies have shown that patients often do not receive enough assistance, due to a lack of stoma care clinics and the difficulty of traveling to the hospital, demonstrating the need for intervention after surgery.

An illustration showing an app being developed by researchers at Mount Sinai would help bladder cancer patients learning to negotiate life with an ostomy.
In a new study, Dr. Mohamed is evaluating the acceptability and feasibility of a web-based program she is developing called MORE (Mobile Ostomates REsources), available on a patient’s computer, mobile phone, or tablet. The program would offer detailed educational modules about stoma site selection and ostomy surgery; instructor-guided sessions on stoma care; and a support component to help patients adapt to their new lifestyle.
The study will include two groups, 24 patients randomly selected to receive the usual care and 48 patients randomly selected to participate in the MORE program before and after surgery. The study results will guide further refinement of MORE for a larger experimental trial. The National Institute of Nursing Research is funding this study.
Team Effort Leads to Successful Renal Autotransplantation
Drawing on their track record of success in renal autotransplantation, a team of Mount Sinai Health System doctors chose this complex, aggressive approach to treat a patient with a history of urological complications and chronic conditions to ensure the best possible outcome for recovery and long-term health.
In fall 2016, Michael Palese, MD, Chair of the Department of Urology at Mount Sinai Downtown and Professor of Urology at the Icahn School of Medicine at Mount Sinai, treated a 64-year-old female patient with a range of medical issues. These included chronic left distal ureteral stricture and a history of recurrent kidney stones. Before coming to Mount
Sinai, the patient had undergone a distal ureteral reimplant with a psoas hitch to address the chronic strictures, but that had not helped her situation. At the time, she had a nephrostomy tube and stents in place. Previous attempts to remove those stents, in combination with recurrent urinary tract infections and kidney stones, had resulted in extensive damage to the patient’s ureter.
Dr. Palese, a leading authority in the research and treatment of kidney disease—specifically kidney cancer and kidney stones—was concerned that the damage to the ureter could limit the blood supply necessary to proceed with a conventional solution, such as the creation of an ileal or buccal mucosa ureter. He believed that laparoscopic renal autotransplantation was the most practical approach because it would enable the patient to keep her kidney and avoid major surgery that could potentially disrupt another organ system. After discussing her options with Dr. Palese, the patient agreed to a renal autotransplant with possible bladder construction.
The surgical team approached the procedure as it would any other donor nephrectomy. After placing the patient in a flank position, Dr. Palese made three tiny laparoscopic incisions in the abdomen, incorporating one for the extraction and replacement of the entire left kidney. Once removed, the kidney appeared perfectly normal, but the tissue around the ureter demonstrated extensive damage and inflammation. The kidney was then prepared, dissected free of surrounding fat and other materials, flushed with a chilled preservative, and placed in an ice bath to await reimplantation.

After Dr. Palese identified an adequate length of quality artery and vein, Sander Florman, MD, the Director of the Recanati/ Miller Transplantation Institute at The Mount Sinai Hospital and the Charles Miller, MD Professor of Surgery at the Icahn School of Medicine, led a surgical team in reimplanting the organ in the patient’s pelvis. It was attached to the left external iliac artery and vein.
“We were able to cut back the diseased ureter to the point where it was healthy, and that enabled us to place the kidney on top of the bladder,” says Dr. Palese, who is also Director
of Minimally Invasive Surgery for the Mount Sinai Health System. “It reperfused well, which was important because that enables healing.”
Dr. Palese says the ureter appeared healthy with good urine output, and the kidney began making urine following an end-to-side ureteroneocystostomy, or ureteral implantation, over a 10 cm double-J stent with running 5-0 PDS® suture. There were no complications, and ultrasound imaging confirmed that the procedure was a success. The patient has not subsequently experienced any strictures, pain, or problems with urinating, according to Dr. Palese.
“This is the outcome we like to see—to be able to give patients back their quality of life without any infections or complications whatsoever,” he says. “Autotransplantation is a very complex and relatively aggressive approach to correcting this very difficult problem. But the reward of a healthy life without any further intervention makes it worthwhile.”
Robotic Surgery Aids in Treatment Of Advanced Bladder Cancer
Combining expertise in robotic surgery and clinical trials with a novel surgical approach, Mount Sinai doctors have demonstrated how innovation in treatment can accomplish a successful result in a patient with advanced bladder cancer.
In December 2015, John Sfakianos, MD, an Assistant Professor of Urology and Urologic Oncology at the Icahn School of Medicine at Mount Sinai, saw an 80-year-old male patient from Pennsylvania. Before being referred to Mount Sinai, the patient had been treated for prostate cancer five years earlier and, more recently, had undergone both a biopsy that revealed muscle-invasive bladder cancer and a CT scan that demonstrated hydronephrosis of the left kidney. Because the tumor prevented the kidney from draining, the patient presented with a nephrostomy tube placed in the left kidney.
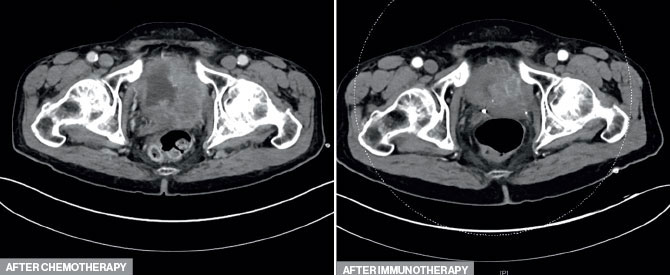
Dr. Sfakianos determined that the best path of treatment was chemotherapy followed by a radical cystectomy. Yet when the patient finished chemotherapy in April 2016, a biopsy revealed that the tumor in his bladder had continued growing and was now invading the right side of his pelvis, making it unresectable. Realizing that a novel approach was necessary to reduce the size of the tumor, Dr. Sfakianos referred the patient to Matthew Galsky, MD, Professor of Medicine (Hematology and Medical Oncology) at the Icahn School of Medicine, and Director of Genitourinary Medical Oncology at The Tisch Cancer Institute. Dr. Galsky had previously played a key role in the clinical trials testing atezolizumab, an immune checkpoint inhibitor, for the treatment of bladder cancer. These trials demonstrated that in a subset of patients with bladder cancer progressing despite chemotherapy, atezolizumab led to tumor shrinkage. The patient initiated atezolizumab and, after 17 treatments, MRIs and CT scans confirmed that the tumor had shrunk to the point where it would be amenable to surgical resection.
Due to the complex nature of this operation, a robotic approach was favored. Ketan Badani, MD, Director of Robotic Surgery and Vice Chair of Urology, was consulted for the robotic approach. “In my opinion, a robotic approach is superior for these complex operations that require exquisite precision and visualization to safely remove the cancer,” Dr. Badani says.
In September 2017, Drs. Badani and Sfakianos worked together to perform the radical cystectomy. “This was a difficult surgery because the area of pelvic sidewall invasion had a lot of fibrosis. However, we were able to remove the bladder with a clean margin,” Dr. Badani says.

Dr. Sfakianos and Dr. Badani used the GelPort laparoscopic system to perform a hybrid extracorporeal/intracorporeal procedure to create a urinary diversion, using 12 cm of small intestines. Once the ileal conduit was completed, a robotic approach was used to reinsert the intestines and connect the ureters to the conduit.
Dr. Sfakianos says the four-and-a-half-hour procedure was also unique in that the patient was anesthetized with quadratus lumborum nerve block using lidocaine and Marcaine. “That is part of a program we have introduced where our patients do not receive narcotics intraoperatively, during anesthesia, or during recovery,” he explains. “The outcomes have been exceptional, as we’ve been able to cut the length of hospital stays by almost half and complications by one-third.”
Apart from an ileus, there were no complications stemming from the surgery, and the final pathology revealed cancer confined to the first layer of the bladder (pT1), according to Dr. Sfakianos. The patient has been doing well since the surgery and will be monitored to ensure that he remains disease free.
Message from the Chair: Ash Tewari, MBBS, MCh
At the Milton and Carroll Petrie Department of Urology at the Icahn School of Medicine at Mount Sinai, we have experienced one of the most exciting periods of growth since I assumed the role of Chair four years ago. This seems fitting, as 2017 marked the 75th anniversary of the Department’s founding.

Our mission continues to include educating the next generation of urologic surgeon-scientists and exchanging discoveries and clinical translations with colleagues throughout the United States and around the world. To that end, we organized two highly successful CME urologic oncology symposia in 2017. First, there was a standing-room-only event in May at the American Urological Association in Boston, featuring 3D viewing and analyses of oncologic robotic surgeries. Then we held our 2nd International Prostate Cancer Symposium and Inaugural World Congress of Urologic Oncology at The Mount Sinai Hospital in New York in September. In total, more than 800 global urology specialists and allied health care professionals attended these events. You can read about the highlights of the September meeting in this report.
As the Icahn School of Medicine at Mount Sinai enters its 50th anniversary year, our faculty are among the leading expert surgeons in the world, and we are proud to present here three of our most recent challenging cases in oncology and renal transplantation. We also showcase the unique behavioral research we have embarked on to assess demand for and compliance with active surveillance treatment for prostate cancer, as well as the often neglected needs of bladder cancer patients learning to negotiate life with an ostomy.
In 2017, we grew our Department by almost 25 percent and expanded patient services by recruiting rising and veteran talent to strengthen and grow our programs in oncology, reconstructive surgery, men’s and women’s health, and transgender medicine.

I am delighted to welcome to our faculty seven renowned physicians. Jerry Blaivas, MD, and Rajveer Purohit, MD, MPH, are reconstructive urologists. Barbara Chubak, MD, is a general urologist with a specialty in male and female sexual dysfunction. Isuru Jayaratna, MD, is a general and oncologic urologist practicing with Mount Sinai Doctors Long Island. Avinash Reddy, MD, works in our midtown office and is a general and urologic oncology specialist. Vannita Simma-Chiang, MD, is a general and female urology specialist. And Cynthia Trop, MD, is a general urologist. Please visit our website, www.mountsinai.org/urology, to meet our faculty teams.
Finally, be sure to save the dates September 6 to 9 for our 2018 Urologic Oncologic Symposium, which will once again be held at The Mount Sinai Hospital. Please contact me if you are interested in attending or joining the Symposium faculty. I would be delighted to chat, and I look forward to seeing you there. You can reach me at ash.tewari@mountsinai.org or 212-241-9955.
Ash Tewari, MBBS, MCh, is the Kyung Hyun Kim, MD Chair in Urology of the Milton and Carroll Petrie Department of Urology.