Histoplasmosis - acute (primary) pulmonary
Acute pulmonary histoplasmosis is a respiratory infection that is caused by inhaling the spores of the fungus Histoplasma capsulatum.
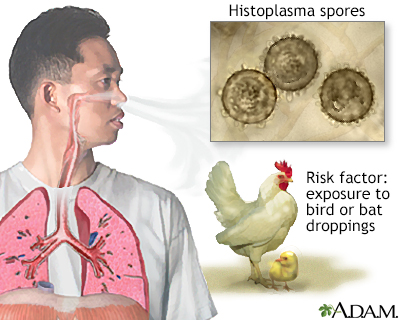
Histoplasmosis is a fungal infection caused by inhaling dust from spore-infected bird droppings. The acute form is treated with antifungal medication.
Fungal infections are caused by microscopic organisms (fungi) that can live on the skin. They can live on the dead tissues of the hair, nails, and outer skin layers.
Causes
Histoplasma capsulatum is the name of the fungus that causes histoplasmosis. It is found in the central and eastern United States, eastern Canada, Mexico, Central America, South America, Africa, and Southeast Asia. It is commonly found in the soil in river valleys. It gets into the soil mostly from bird and bat droppings.
You can get sick when you breathe in spores that the fungus produces. Every year, thousands of people with a normal immune system worldwide are infected, but most do not become seriously sick. Most have no symptoms or have only a mild flu-like illness and recover without any treatment.
Acute pulmonary histoplasmosis may happen as an epidemic, with many people in one region becoming sick at the same time. People with weakened immune systems (see Symptoms section below) are more likely to:
- Develop the disease if exposed to the fungus
- Have the disease come back
- Have more symptoms, and more serious symptoms, than others who get the disease
Risk factors include traveling to or living in the central or eastern United States near the Ohio and Mississippi river valleys and being exposed to the droppings of birds and bats. This threat is greatest after an old building is torn down and spores get into the air, or when exploring caves.
Symptoms
Most people with acute pulmonary histoplasmosis have no symptoms or only mild symptoms. The most common symptoms are:
- Chest pain
- Chills
- Cough
- Fever
- Joint pain and stiffness
- Muscle aches and stiffness
- Rash (usually small sores on the lower legs)
- Shortness of breath
Acute pulmonary histoplasmosis can be a serious illness in the very young, older people, and people with a weakened immune system, including those who:
- Have HIV/AIDS
- Have had bone marrow or solid organ transplants
- Take medicines that suppress their immune system
Symptoms in these people may include:
- Inflammation around the heart (called pericarditis)
- Serious lung infections
- Severe joint pain
Exams and Tests
To diagnose histoplasmosis, you must have the fungus or signs of the fungus in your body. Or your immune system must show that it is reacting to the fungus.
Tests include:
- Antibody tests for histoplasmosis
- Biopsy of infection site
- Bronchoscopy (usually only done if symptoms are severe or you have an abnormal immune system)
- Complete blood count (CBC) with differential
- Chest CT scan
- Chest x-ray (might show a lung infection or pneumonia)
- Sputum culture (this test often does not show the fungus, even if you are infected)
- Urine test for Histoplasma capsulatum antigen
Treatment
Most cases of histoplasmosis clear up without specific treatment. People are advised to rest and take medicine to control fever.
Your health care provider may prescribe medicine if you are sick for more than 4 weeks, have a weakened immune system, or are having breathing problems.
Outlook (Prognosis)
When histoplasmosis lung infection is severe or gets worse, the illness may last up to many months. Even then, it is rarely fatal.
The illness can get worse over time and become a long-term (chronic) lung infection (which doesn't go away).
Possible Complications
Histoplasmosis can spread to other organs through the bloodstream (dissemination). This is often seen in infants, young children, and people with a suppressed immune system.
When to Contact a Medical Professional
Contact your provider if:
- You have symptoms of histoplasmosis, especially if you have a weakened immune system or have recently been exposed to bird or bat droppings
- You are being treated for histoplasmosis and develop new symptoms
Prevention
Avoid contact with bird or bat droppings if you are in an area where the spore is common, especially if you have a weakened immune system.
References
Deepe GS. Histoplasma capsulatum (histoplasmosis). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 263.
Thompson GR, Miceli MH. Endemic mycoses. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 308.
Version Info
Last reviewed on: 3/16/2024
Reviewed by: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
