Pneumonia - weakened immune system
Pneumonia in immunodeficient patient; Pneumonia - immunocompromised host; Cancer - pneumonia; Chemotherapy - pneumonia; HIV - pneumonia
Pneumonia is a lung infection. It can be caused by many different germs, including bacteria, viruses, and fungi.
This article discusses pneumonia that occurs in a person who has a hard time fighting off infection because of problems with the immune system. This type of disease is called "pneumonia in an immunocompromised host."
Related conditions include:
- Hospital-acquired pneumonia
- Pneumocystis jiroveci (previously called Pneumocystis carinii) pneumonia
- Pneumonia cytomegalovirus
- Fungal pneumonia
- Pneumonia
- Viral pneumonia
- Walking pneumonia
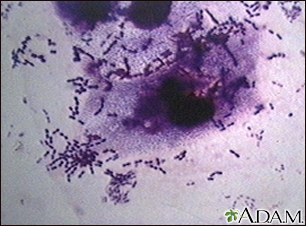
This picture shows the organism Pneumococci. These bacteria are usually paired (diplococci) or appear in chains. Pneumococci are typically associated with pneumonia, but may cause infection in other organs such as the brain (pneumococcal meningitis) and blood stream (pneumococcal septicemia). (Image courtesy of the Centers for Disease Control and Prevention.)
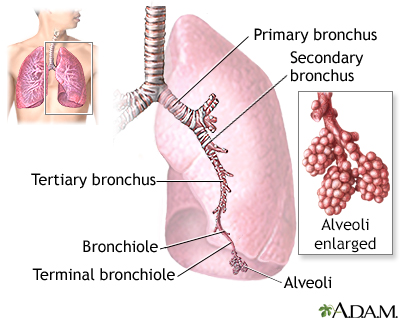
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
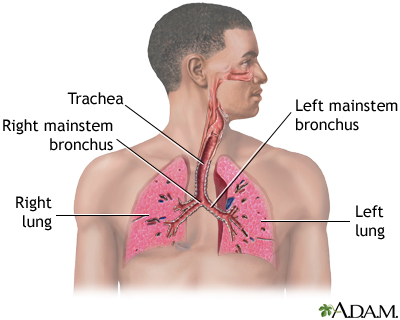
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Causes
People whose immune system is not working well are less able to fight off germs. This makes them prone to infections from germs that do not often cause disease in healthy people. They are also more vulnerable to regular causes of pneumonia, which can affect anyone.
Your immune system may be weakened or not work well because of:
- Bone marrow transplant
- Chemotherapy
- HIV infection
- Leukemia, lymphoma, and other conditions that harm your bone marrow
- Autoimmune disorders
- Medicines (including steroids, and those used to treat cancer and control autoimmune diseases)
- Organ transplant (including kidney, heart, and lung)
Symptoms
Symptoms may include:
- Cough (may be dry or produce mucus-like, greenish, or pus-like sputum)
- Chills with shaking
- Fatigue
- Fever
- General discomfort, uneasiness, or ill feeling (malaise)
- Headache
- Loss of appetite
- Nausea and vomiting
- Sharp or stabbing chest pain that gets worse with deep breathing or coughing
- Shortness of breath
Other symptoms that may occur:
- Heavy sweating or night sweats
- Stiff joints (rare)
- Stiff muscles (rare)
Exams and Tests
Your health care provider may hear crackles or other abnormal breath sounds when listening to your chest with a stethoscope. Decreased volume of breath sounds is a key sign. This finding may mean there is a buildup of fluid between the chest wall and lung (pleural effusion).
Tests may include:
- Arterial blood gases
- Blood chemistries
- Blood culture
- Bronchoscopy (in certain cases)
- Chest CT scan (in certain cases)
- Chest x-ray
- Complete blood count
- COVID test
- Lung biopsy (in certain cases)
- Serum cryptococcus antigen test
- Serum galactomannan test
- Galactomannan test from bronchial alveolar fluid
- Sputum culture
- Sputum Gram stain
- Sputum immunofluorescence tests (or other immune tests)
- Urine tests (to diagnose Legionnaire's disease or Histoplasmosis)
Treatment
Antibiotics or antifungal medicines may be used, depending on the type of germ that is causing the infection. Antibiotics are not helpful for viral infections, but newer medicines may treat some viral infections for example COVID-19. You may need to stay in the hospital during the early stages of the illness.
Oxygen and treatments to remove fluid and mucus from the respiratory system are often needed.
Outlook (Prognosis)
Factors that may lead to a worse outcome include:
- The pneumonia that is caused by a fungus.
- The person has a very weak immune system.
Possible Complications
Complications may include:
- Respiratory failure (a condition in which a patient can't take in oxygen and get rid of carbon dioxide without the use of a machine to deliver breaths.)
- Sepsis
- Spread of the infection
- Death
When to Contact a Medical Professional
Contact your provider if you have a weakened immune system and you have symptoms of pneumonia.
Prevention
If you have a weakened immune system, you may receive daily antibiotics to prevent some types of pneumonia.
Ask your provider if you should receive the influenza (flu), pneumococcal (pneumonia), and COVID-19 vaccines.
Practice good hygiene. Thoroughly wash your hands with soap and water:
- After being outdoors
- After changing a diaper
- After doing housework
- After going to the bathroom
- After touching body fluids, such as mucus or blood
- After using the telephone
- Before handling food or eating
Other things you can do to reduce your exposure to germs include:
- Consider wearing a face mask when outside of your house.
- Keep your house clean.
- Stay away from crowds.
- Ask visitors who have a cold to wear a mask or not to visit.
- Do not do yard work or handle plants or flowers (they can carry germs).
References
Blijlevens NMA, van der Velden WJFM. Infections in the immunocompromised host: general principles. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 305.
Perkins J, Waasdorp CP. The immunocompromised patient. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 182.
Sifri CD, Marr KA. Approach to fever and suspected infection in the immunocompromised host. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 265.
Wunderink RG, Restrepo MI. Pneumonia: considerations for the critically ill. In: Parrillo JE, Dellinger RP, eds. Critical Care Medicine: Principles of Diagnosis and Management in the Adult. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 40.
Version Info
Last reviewed on: 5/19/2023
Reviewed by: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
