Abdominal sounds
Bowel sounds
Abdominal sounds are the noises made by the intestines.
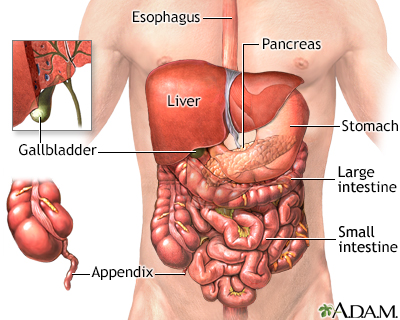
The process of digesting food is accomplished by many organs in the body. Food is pushed by the esophagus into the stomach. The stomach mixes the food and begins the breakdown of proteins. The stomach propels the food then into the small intestine. The small intestine further digests food and begins the absorption of nutrients. Secretions from the pancreas in the small intestine help neutralize the acid in the intestine to provide a proper environment for the enzymes to function. Bile from the gallbladder and liver emulsify fat and enhance the absorption of fatty acids. The large intestine temporarily stores and concentrates the remainder until it is passed out as waste from the body.

Living with ulcerative colitis can be a constant gamble. You run to the grocery store, hoping this won't be the day when your disease flares up. You might get lucky, or your disease could hit again in the middle of the store, leaving you in a search for a bathroom. Let's talk about ulcerative colitis. Ulcerative colitis is a type of inflammatory bowel disease. It's caused by a malfunction in the body's immune system. Normally, the immune system protects against bacteria and other foreign invaders. But in people with ulcerative colitis, it mistakenly attacks the rectum and intestines, causing them to swell up and thicken. As a result, people with ulcerative colitis have bouts of severe abdominal pain and diarrhea. They can lose weight without meaning to. If you've been experiencing any of these symptoms, your doctor can test for ulcerative colitis with a colonoscopy. Your doctor can take a sample of your intestines, to diagnose ulcerative colitis and check for colon cancer, a risk associated with ulcerative colitis. Medicines can help with the symptoms of ulcerative colitis. There are medicines to control diarrhea, and pain relievers to help with the abdominal cramps. There are also medicines that quiet the overactive immune response that causes ulcerative colitis. Changing your diet may help control your immune system from attacking your intestines. Changing your diet can limit diarrhea and gas, especially when you're having active attacks. Your doctor may recommend you eat small meals throughout the day, drink plenty of water, and avoid high-fiber foods and high-fat foods. You may feel worried, embarrassed, or even sad or depressed about having bowel accidents. Other stressful events in your life, such as losing a job or a loved one, may make your symptoms worse. Your doctor can help you manage your stress. If your symptoms are severe, surgery to remove your large intestine may be the best way to cure your ulcerative colitis. If you're experiencing any ulcerative colitis symptoms-like stomach pain, diarrhea, or unplanned weight loss, call your doctor. Although surgery is the only cure, treatments can relieve some of the uncomfortable symptoms, and help you to lead a more normal life-free from the constant stress of having to search for the bathroom.
Considerations
Abdominal sounds (bowel sounds) are made by the movement of the intestines as they push food through. The intestines are hollow, so bowel sounds echo through the abdomen much like the sounds heard from water pipes.
Most bowel sounds are normal. They simply mean that the gastrointestinal tract is working. However, there are some cases in which abnormal sounds can indicate a problem. A health care provider can check abdominal sounds by listening to the abdomen with a stethoscope (auscultation).
Ileus is a condition in which there is a lack of intestinal activity. Many medical conditions may lead to ileus. This problem can cause gas, fluids, and the contents of the intestines to build up and break open (rupture) the bowel wall. The provider may be unable to hear any bowel sounds when listening to the abdomen.
Reduced (hypoactive) bowel sounds include a reduction in the loudness, tone, or regularity of the sounds. They are a sign that intestinal activity has slowed.
Hypoactive bowel sounds are normal during sleep. They also occur normally for a short time after the use of certain medicines and after abdominal surgery. Decreased or absent bowel sounds often indicate constipation.
Increased (hyperactive) bowel sounds can sometimes be heard even without a stethoscope. Hyperactive bowel sounds mean there is an increase in intestinal activity. This may happen with diarrhea or after eating.
Abdominal sounds are always evaluated together with symptoms such as:
- Gas
- Nausea
- Presence or absence of bowel movements
- Vomiting
If bowel sounds are hypoactive or hyperactive and there are other abnormal symptoms, you should continue to follow-up with your provider.
For example, no bowel sounds after a period of hyperactive bowel sounds can mean there is a rupture of the intestines, or strangulation of the bowel and death (necrosis) of the bowel tissue.
Very high-pitched bowel sounds may be a sign of early bowel obstruction.
Causes
Most of the sounds you hear in your stomach and intestines are due to normal digestion. They are not a cause for concern. Many conditions can cause hyperactive or hypoactive bowel sounds. Most are harmless and do not need to be treated.
The following is a list of more serious conditions that can cause abnormal bowel sounds.
Hyperactive, hypoactive, or missing bowel sounds may be caused by:
- Blocked blood vessels prevent the intestines from getting proper blood flow. For example, blood clots can cause mesenteric artery occlusion.
- Mechanical bowel obstruction is caused by hernia, tumor, adhesions, or similar conditions that can block the intestines.
- Paralytic ileus is a problem with the nerves to the intestines.
Other causes of hypoactive bowel sounds include:
- Medicines that slow down movement in the intestines such as opioids (including codeine), anticholinergics, and phenothiazines
- General anesthesia
- Radiation to the abdomen
- Spinal anesthesia
- Surgery in the abdomen
Other causes of hyperactive bowel sounds include:
When to Contact a Medical Professional
Contact your provider if you have any symptoms such as:
- Bleeding from your rectum
- Nausea
- Diarrhea or constipation that continues
- Vomiting
What to Expect at Your Office Visit
The provider will examine you and ask you questions about your medical history and symptoms. You may be asked:
- What other symptoms do you have?
- Do you have abdominal pain?
- Do you have diarrhea or constipation?
- Do you have abdominal distention?
- Do you have excessive or absent gas (flatus)?
- Have you noticed any bleeding from the rectum or black stools?
You may need the following tests:
- Abdominal CT scan
- Abdominal x-ray
- Blood tests
- Endoscopy
If there are signs of an emergency, you will be sent to the hospital. A tube may be placed through your nose or mouth into the stomach or the upper intestine. This empties your stomach or upper intestine. In most cases, you will not be allowed to eat or drink anything so your intestines can rest. You will be given fluids through a vein (intravenously).
You may be given medicine to reduce symptoms and to treat the cause of the problem. The type of medicine will depend on the cause of the problem. Some people may need surgery right away.
References
Ball JW, Dains JE, Flynn JA, Solomon BS, Stewart RW. Abdomen. In: Ball JW, Dains JE, Flynn JA, Solomon BS, Stewart RW, eds. Seidel's Guide to Physical Examination. 10th ed. St Louis, MO: Elsevier; 2023:chap 18.
Landmann A, Bonds M, Postier R. Acute abdomen. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 46.
McQuaid KR. Approach to the patient with gastrointestinal disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 118.
Version Info
Last reviewed on: 10/9/2024
Reviewed by: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
