Researchers Reveal That the Sympathetic Nervous System, not White Blood Cells, is Critically Important in the Regulation of Energy Expenditure and Thermogenesis
A new study from the Icahn School of Medicine at Mount Sinai provides important insights into how the body regulates its production of heat, a process known as thermogenesis that is currently intensely studied as a target of diabetes and obesity treatment in humans.
While researchers had previously hypothesized that macrophages, a class of white blood cells, played a major role in thermogenesis, the new study suggests that the main driver of thermogenesis is the sympathetic nervous system, which is chiefly controlled by the brain. The results were published online today in Nature Medicine.
The Mount Sinai research team led by Christoph Buettner, MD, PhD, senior author of the study and Professor of Medicine (Endocrinology, Diabetes, and Bone Disease) at the Icahn School of Medicine at Mount Sinai, focused on catecholamines, hormones released by the sympathetic nervous system to activate brown fat tissue. Brown adipose tissue is a type of fat tissue that burns energy to produce heat and keep us warm. Catecholamines can also convert white fat tissue, the more familiar kind of fat tissue that stores lipids, into a tissue that resembles brown fat. The researchers tested whether macrophages could provide an alternative source of catecholamines, as had been proposed in recent years.
“Thermogenesis is a metabolic process that receives a lot of interest as a target of drugs that allow you to burn energy and hence reduce obesity and improve diabetes. It turns out that macrophages are not that important, as they are unable to make catecholamines, but clearly the brain through the sympathetic nervous system is,” says Dr. Buettner. “Therefore, it is very important to study the role of the brain and the sympathetic nervous system when it comes to understanding metabolism.”
The ability to generate heat is critical for the survival of warm-blooded animals, including humans, as it prevents death by hypothermia. “This evolutionary pressure shaped the biology of humans and that of other warm-blooded animals, and may in part explain why humans are susceptible to developing diabetes in the environment in which we live,” says Dr. Buettner.
According to Dr. Buettner, while a lot of effort has been invested in targeting the immune system to cure diabetes and insulin resistance, as of yet there are no anti-inflammatory drugs that have been shown to work well in humans with metabolic disease. “Our study suggests that perhaps the key to combating the devastating effects of diabetes and obesity in humans is to restore the control of thermogenesis and metabolism by the brain and the autonomic nervous system,” says Dr. Buettner.
This study was performed collaboratively between Mount Sinai and eight other institutions from around the world, most prominently with the group of Timo D. Müller, PhD, Institute for Diabetes and Obesity at the Helmholtz Center Munich in Germany.
This work was further supported by grant from the German Research Foundation DFG-TS226/1-1, DFG-TS226/3-1,SFB1123, Nutripathos Project ANR-15-CE14-0030, European Research Council ERC AdG HypoFlam no. 695054 (to M.H.T.); DFG He3260/8-1, the EU FP7 Network “DIABAT,” the EU ITN Network “TRAIN” 721531 (to S.H.); NIH R01AA023416, DK082724 and a career-development award from the American Diabetes Association (to C.B.); NIH R01DK099222 (to S.D.); NIH DK17844 (to S.C.W.); the Israeli Science Foundation and European Research Council (AdvERC grant 340345) (to S.J.) and the Swedish Research Council and the Knut and Alice Wallenberg Foundation (to J.N. and B.C.).
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
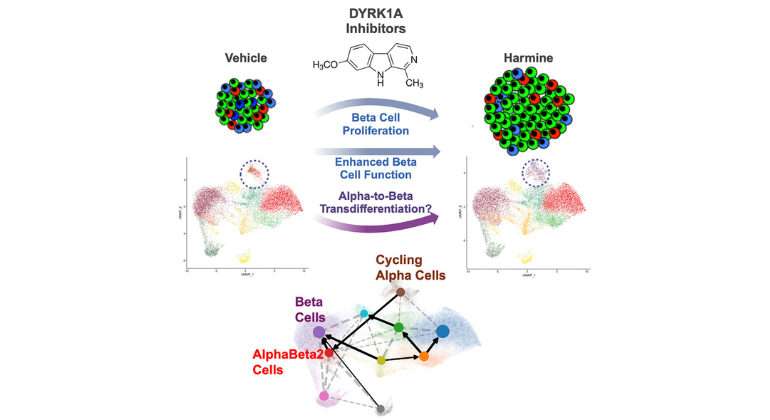
Mount Sinai Researchers Move Closer to a Cure for Diabetes
Dec 10, 2024 View All Press Releases
Diabetes May Accelerate Blood Cancer Growth, Yet Survival Outcomes Differ by Race
Sep 29, 2023 View All Press Releases
Researchers Identify Potential Target for Treatment Among Patients With Type 2 Diabetes
Aug 04, 2022 View All Press Releases