Mount Sinai Ophthalmologists Develop New Technique to Assess Progression of Sickle Cell Retinopathy
Breakthrough technology may help prevent vision loss and understand effectiveness of therapy
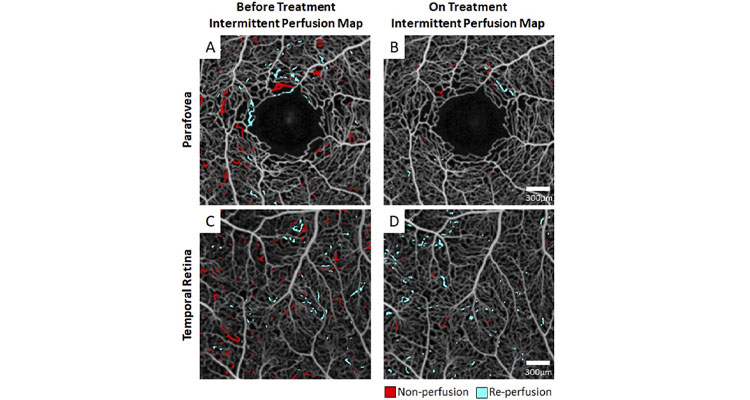
A treatment naïve SCD patient with HbSS genotype was imaged at an initial visit (left column) and repeated imaging again after two months of hydroxyurea treatment (right column). Before treatment, the patient exhibited between-session IPI of 3.0% and 2.7% respectively at the parafovea (A) and temporal retina (C). After two months of hydroxyurea, the between-session IPI was reduced to 0.5% and 1.6% respectively at the parafovea (B) and temporal retina (D).
Ophthalmologists at New York Eye and Ear Infirmary of Mount Sinai have created a new technique to evaluate patients with sickle cell retinopathy and assess the disease before it progresses and leads to permanent vision loss.
Using optical coherence tomography (OCT) angiography—an advanced imaging system that captures the motion of red blood cells in blood vessels non-invasively—the researchers discovered that sequential imaging of affected retinal blood flow in sickle cell patients can help assess how the disease is progressing and how effective their treatment is for reducing focal vascular strokes. Their study was published in the online May issue of Biomedical Optics Express.
“We have added a new dimension to ocular imaging technology that no one has thought of before. For the first time, we have shown that by doing rapid, repeated retinal imaging of sickle cell patients, you can see microscopic changes in blood vessels and blood flow. The more the blood flow fluctuates across images, the more at risk patients are for a permanent blockage, which severely damage their eyesight,” says lead investigator Toco Chui, PhD, Director of the Marrus Adaptive Optics Laboratory at New York Eye and Ear Infirmary of Mount Sinai. “Using this approach, we can non-invasively monitor the retina over time and see how a patient is doing before or after initiation of therapy.”
Sickle cell disease is an inherited red blood cell disorder caused by a mutation in hemoglobin. The hemoglobin folds abnormally and distorts red blood cells into a sickle shape; the sickle-shaped cells clump together and can block blood flow. This causes repeated damage to capillaries, which become inflamed and sticky, resulting in permanent blockages that can affect vision in the retina, and in some cases, major bleeding and retinal detachment.
“Our work can be a game-changer for sickle cell patients, especially for those who have no symptoms of retinopathy. It can lead to earlier diagnosis of retinal issues and prevention of irreversible blindness. Without this technology, it’s impossible to judge their eye condition until patients report vision loss, when it’s too late,” says co-author Richard Rosen, MD, Belinda Bingham Pierce and Gerald G. Pierce, MD Distinguished Chair of Ophthalmology, and Chief of Retina Services for the Mount Sinai Health System.
The researchers analyzed 27 participants. Thirteen had sickle cell disease with retinopathy of varying severity levels; some were on standard therapy (hydroxyurea) and others were not on treatment. The remaining 14 were controls, with no sickle cell disease or retinopathy. The team used OCT angiography to image all subjects 10 times in a row over a 10-minute span. An hour later they repeated the imaging procedure. They analyzed the blood vessels that repeatedly opened and closed—a trait of sickle cell disease. When this happens, blood cannot flow freely and these blood vessels are at risk of permanent closure which can lead to blindness. For patients without sickle cell disease, scans showed that the blood vessels for the most part remained open, providing continuous blood flow.
For each patient, researchers stacked their groups of ten scans together and counted the blood vessels that “flickered.” Healthy blood vessels remain white on all scans with no flickering, indicating consistent blood flow in the vessels. On all scans, the untreated sickle cell patients had substantially more flickering (more intermittent blood flow) than patients on treatment, indicating that treatment was effective. Patients with no sickle cell disease had no or very minimal blood flow fluctuations. Investigators used measurements of flicker frequency and locations of flickering to develop a computer algorithm for assessing risk of retinal blood blockages in sickle cell patients.
“For the first time ever in sickle cell disease, we have too many good drugs and we don't know well enough who should be on what, and what combinations work best. What we hope is that OCT angiography and this new algorithm can be used to solve this problem. Instead of following lab tests and waiting for horrible things to happen to the patient, for the first time we can use this technology to measure the number of vaso-occlusive events that are occurring on a new treatment regimen to find out if it is best for the patient,” says Jeffery Glassberg, MD, Director of the Director of Mount Sinai’s Comprehensive Sickle Cell Program.
Davis B. Zhou, a medical student from the Icahn School of Medicine at Mount Sinai, played an integral role in creating the algorithm for the study during his extended research elective in the Einhorn Center for Clinical Research at the New York Eye and Ear Infirmary of Mount Sinai.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
Blinding Eye Disease Strongly Associated With Serious Forms of Cardiovascular Disease
Nov 17, 2022 View All Press Releases
High-Tech Imaging Offers New Way to Detect Signs of Early Glaucoma
Aug 02, 2022 View All Press Releases
Blinding Eye Disease Is Strongly Associated With Heart Disease and Stroke
Jul 12, 2022 View All Press ReleasesMount Sinai Recruits Internationally Recognized Ophthalmologists to Expand Leadership
Dec 17, 2018 View All Press Releases