Care More Expensive for Dementia Patients and Families in Last Years of Life
The cost of care over the last five years of life for patients with dementia is significantly higher than for patients who die from heart disease, cancer, or other causes, according to a study led by researchers at the Icahn School of Medicine at Mount Sinai, Dartmouth College and University of California, Los Angeles, and published online today in the journal Annals of Internal Medicine. The study was funded by the National Institute on Aging.
In addition to higher total end-of-life costs, the study found that out-of-pocket spending for patients with dementia was 81 percent higher than for those who died from other causes. The burden of this spending, measured as the proportion of household wealth devoted to out-of-pocket costs, was particularly high for dementia patients who were black, had less than a high school education, or were unmarried or widowed women.
This is the first national study which looks at total costs (patient and family expenses, as well as Medicare and Medicaid expenditures) over the last five years of life for those with dementia in comparison to those without, according to the study authors. It also estimated the cost of family caregiving for patients with dementia, which is defined as a decline in mental ability severe enough to interfere with daily life. Symptoms can include memory loss, as well as declines in language, problem-solving and other cognitive skills. People with Alzheimer’s Disease represent the majority of dementia cases.
“Our study shows that all households, regardless of disease, face substantial financial risks during the last years of life; however, households of those with dementia face an even greater burden of costs, particularly with regard to out-of-pocket expenses and the costs of caregiving,” said Amy Kelley, MD, Associate Professor of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai and lead author of the study. “Many costs related to daily care for patients with dementia are not covered by health insurance, and these care needs--from supervision, to bathing and feeding--may span several years.
While Medicare provides nearly universal coverage for U.S. adults over age 65, it does not cover health-related expenses most valuable to those with chronic diseases or a life-limiting illness, such as homecare services, equipment and non-rehabilitative nursing home care. People living with dementia often face many years of progressive functional decline and require long-term, supportive care.
Researchers analyzed data from 1,702 Medicare beneficiaries, aged 70 years or older, who died between 2005 and 2010. The group was then subdivided into four main categories: individuals with high probability of dementia, and individuals who died of heart disease, cancer, or other causes. Findings indicated the average total cost for deceased patients with dementia was $287,038 in the last five years of life. This was significantly higher than for those who died of heart disease ($175,136), cancer ($173,383), or other causes ($197,286).
“The families of patients with dementia have more expenses than other families, and the financial burden is greatest among families that may be least able to manage it,” said Dr. Kelley. “The discussion of healthcare reform must include the significant uninsured care needs of older adults with dementia and examine ways to mitigate the financial risk currently faced by Medicare beneficiaries.”
The study was supported by the National Institute on Aging. The study’s data was supplied by the Health and Retirement Study (HRS), a national sample of U.S. adults age 50 linked to Medicare claims. The HRS includes detailed information on out-of-pocket spending and total Medicare spending, as well as information about insurance coverage, socioeconomic status, health and cognitive status, and cause of death.
Collaborators of the study include researchers from the Geriatric Research Education and Clinical Centers at the James J Peters VA Medical Center, the University of California Los Angeles Department of Economics, Dartmouth College Department of Economics and The Dartmouth Institute for Health Policy and Clinical Practice at the Dartmouth Medical School.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, employing 48,000 people across its hospitals and more than 400 outpatient practices, as well as more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 11 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2024-2025.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
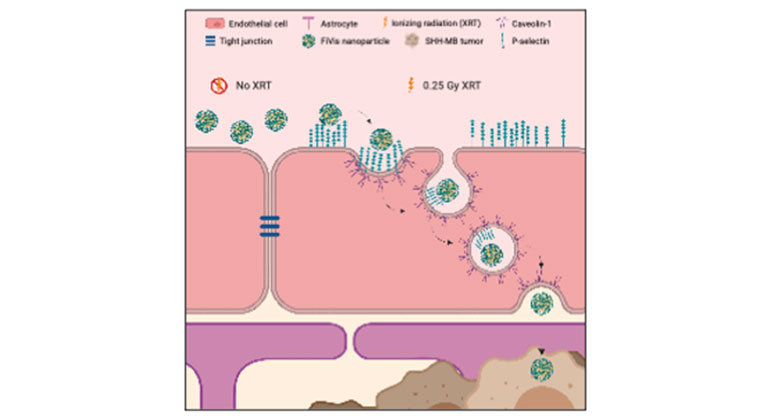
Scientists Develop Novel Approach to Enhance Drug Delivery for Brain Tumors in Children
Mar 02, 2023 View All Press Releases
Researchers Identify the Role of an Alzheimer’s Disease Risk Gene in the Brain
Nov 30, 2022 View All Press Releases