The History of The Mount Sinai Hospital
On January 15, 1852, nine men representing a variety of Jewish charities agreed on a vision for free medical care for indigent Jews in New York City. In 1855, that vision came to fruition with the establishment of the 45-bed Jews' Hospital in New York in what was then a rural neighborhood on West 28th Street between Seventh and Eighth Avenues.
Although the hospital was a sectarian institution, the Jews' Hospital accepted emergency patients of any religious affiliation. In its first years of operation, the majority of patients were foreign born. As the Jews' Hospital was a charitable enterprise, its directors relied on the gifts of friends and members, as well as later payments from the government, to provide enough to subsidize care.
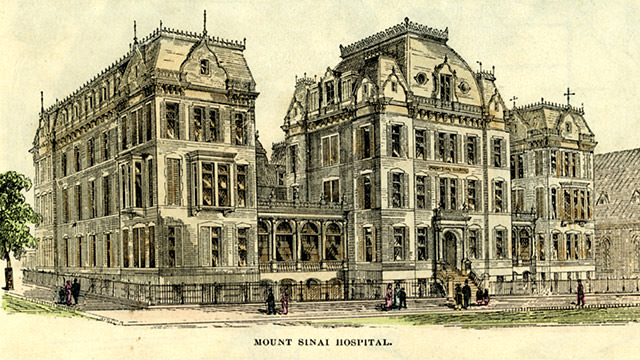
During the Civil War, the hospital expanded to accommodate Union soldiers. After this, to reflect its broadened mission and to ensure its eligibility for state and city support, the Jews' Hospital formally abandoned its sectarian charter in 1866 and was renamed The Mount Sinai Hospital. In 1872, it moved to a new 120-bed facility on Lexington Avenue, between 66th and 67th Streets, nearly tripling its original capacity.
Move to Upper East Side Leads to Expanded Services
With the move to Lexington Avenue, patient care grew to encompass outpatient services as well as new specialties such as pediatrics, eye and ear, neurology, genitourinary, and dermatology. The first tiny laboratory, large enough for only two people, was set up in a coat closet, and from here research took on increased importance.
In 1881, a training school for nurses was established, introducing professional nursing care to a facility previously served by untrained male and female attendants. The Mount Sinai Hospital School of Nursing closed in 1971 after graduating 4,700 nurses.
As advances in research, diagnosis, and patient care occurred, more people sought treatment at hospitals, and Mount Sinai’s leaders realized it was time, once again, to move and expand.
New Facilities on Fifth Avenue Offer Further Growth
In 1904, the new 456-bed, 10-pavilion Mount Sinai Hospital was dedicated on Fifth Avenue at 100th Street. The President of the hospital, Isaac Wallach, described The Mount Sinai Hospital as “this House of noble deeds” with a three-fold mission of “benevolence, science, and education.” Over the years, the hospital has expanded rapidly both physically and in terms of service, becoming a full-service medical facility capable of treating complex conditions. In an effort to help the hospital’s patients balance their medical and social needs, a department of Social Work Services was created in 1907. The latter is supported by the Auxiliary Board, which was formed in 1916 to provide financial support and labor resources to social service-related activities at the Hospital. The Auxiliary today works diligently to support vital hospital and community outreach projects.
Mount Sinai Active in Both World Wars
The Mount Sinai Hospital sent medical units to both World Wars. Of the 24 physicians and 65 nurses serving in World War I with Base Hospital No. 3 of the U.S. Army Medical Corps in France, the majority of doctors and nurses were from The Mount Sinai Hospital. The group finished the conversion of a 15th century monastery in Vauclaire, Dordogne into a 500-bed hospital that at one point housed 2,800 patients.
During World War II, nearly 900 physicians, nurses, staff members and trustees from The Mount Sinai Hospital saw wartime service. The affiliated unit, the U.S. Army 3rd General Hospital, served in North Africa, Italy, and France. Nine people associated with Mount Sinai died while serving.
School of Medicine Opens in 1968
In the late 1950s, the hospital began plans to establish its own medical school, an unusual move for a hospital. With its chartering in 1963, Mount Sinai School of Medicine, now called the Icahn School of Medicine at Mount Sinai, became the first medical school to grow out of a non-university in more than 50 years. The fact that the hospital was encouraged to found a school is a testament to its tradition of excellence in patient care as well as research.
Mount Sinai School of Medicine opened in 1968 in affiliation with The City University of New York. In building the medical school, trustees envisioned a new kind of medical institution—a university of the health sciences. This new institution would encompass a medical school supported by a strong teaching hospital, a graduate school of biological sciences, a graduate school of physical sciences, and undergraduate programs for allied health workers.
The first class in the newly formed Mount Sinai School of Medicine consisted of 36 students, four of whom were women. There were also 23 students in a third year class and 19 students in the Graduate School of Biological Sciences. In 2007, the school began accepting 140 students in each first year class and there are now more than 300 graduate students at any point in time.
The 21st Century
The opening years of the 21st century found The Mount Sinai Medical Center struggling financially, but by the end of the hospital’s 150th anniversary celebration in 2002, steps had already been taken to chart a new course. In January 2003, Kenneth L. Davis, MD, Mount Sinai Class of 1973, was named Dean of the School of Medicine. On March 24th, he was also named President and CEO of the Mount Sinai Medical Center. Four years later, the two offices were split and Dennis S. Charney, MD became Dean of the School of Medicine.
More than 160 years after its founding, The Mount Sinai Hospital continues to grow and lead, fulfilling its commitment to high-quality patient care and teaching conducted in an atmosphere of social concern and scholarly inquiry into the nature, causation, prevention and therapy of human disease.
The Mount Sinai Hospital Firsts
The Mount Sinai Hospital and the Icahn School of Medicine at Mount Sinai have achieved international acclaim for its lengthy list of firsts in research, education, and patient care. Among those firsts include:
Present to 1986
2025—First histotripsy of liver tumors and robotic central pancreatectomy performed.
2024—The Urology Department marks its 500th robotic cystectomy surgery, underscoring its leadership in minimally invasive bladder cancer treatments.
2024—The Mount Sinai Mammovan, a mobile mammography unit, completes its 1,000th breast cancer screening event, delivering more than 10,000 screenings across New York City.
2023—Mount Sinai's cardiovascular surgery team, led by Ismail El-Hamamsy, MD, PhD, performs 100 successful Ross procedures within a single year, a first in the field.
2021—A team of Mount Sinai surgeons led by Eric Genden, MD, performs the world’s first tracheal transplant using donor tissue, offering new hope for patients with airway disease.
2021—Mount Sinai launches the Department of Artificial Intelligence and Human Health, the first of its kind in a U.S. medical school.
2020—The Institute for Health Equity Research is established to better understand health issues affecting communities across all ages, genders, and abilities.
2020—Florian Krammer, PhD, and Viviana Simon, MD, PhD, lead a team that develops, validates, and launches a test that detects the quantity as well as the presence or absence of antibodies to SARS-CoV-2.
2020—The first confirmed COVID-19 case in New York City is diagnosed at The Mount Sinai Hospital by emergency physician Angela Chen, MD, marking the beginning of the COVID-19 pandemic in New York.
2019—Researchers led by Joshua Brody, MD, and Linda Hammerich, PhD, developed a novel approach to cancer immunology, injecting immune stimulants directly into a tumor to teach the immune system to destroy it.
2019—William Oh, MD, and Emanuela Taioli, MD, PhD, lead a research team that finds a link between exposure to dust from the World Trade Center terrorist attack and prostate cancer.
2018— South Nassau Communities Hospital joins the Mount Sinai Health System, expanding services to Long Island communities.
2018—Normal immune cells called macrophages help early breast cancer cells move to other parts of the body, potentially creating metastasis before a tumor has even developed, researchers led by Julio Aguirre-Ghiso, PhD, find.
2018—Two strains of human herpesvirus are found in the brains of people with Alzheimer’s disease at levels up to twice as high as in those without Alzheimer’s, as shown by Joel Dudley, PhD, and Samuel Gandy, MD, PhD.
2017—An “immune map” of the cells and cytokines involved in the development of atopic dermatitis is created by Emma Guttman, MD, PhD, leading to FDA approval of a breakthrough treatment.
2017—Immune cells start to be dysfunctional very early during tumor formation, suggesting that immunotherapy can be effective much earlier than previously believed, researchers led by Miriam Merad, MD, PhD, show.
2017—Mount Sinai psychiatry researchers link strong working memory networks to better physical endurance and cognitive function—marking the first study to connect working memory with overall health and lifestyle.
2017—Researchers at The Tisch Cancer Institute show for the first time how signals in primary head, neck, and breast tumors pre-program cancer cells to become dormant and resist chemotherapy. In a large population study that was the first of its kind, researchers found that a simple tool not requiring laboratory tests, the Fuster-BEWAT score, is as effective as the American Heart Association-recommended ICHS (Ideal Cardiovascular Health Index), which includes blood analysis of cholesterol and glucose. The Fuster-BEWAT score evaluates five health indicators: blood pressure, physical activity, body-mass index, fruit and vegetable intake, and smoking status, and does not require a blood test. These results demonstrate the usefulness of the Fuster-BEWAT score as an index of subclinical atherosclerosis.
2017—Mount Sinai researchers find that 3D vascular ultrasound enhances patient risk stratification by measuring plaque burden in cubic millimeters.
2017—Cardiologists perform the first study using a novel vector for gene therapy to improve heart function in non-ischemic heart failure, showing that gene therapy is now a viable option for treating congestive heart failure.
2017—Mount Sinai and Memorial Sloan Kettering scientists develop the first mathematical model to predict cancer patient response to immunotherapy and identify new immune targets.
2017—Scientists at Mount Sinai, Sema4, and partners create the first predictive model of IBD using a multi-omics approach to map immune-related biological networks.
2017—Mount Sinai microbiology researchers uncover how influenza A hijacks the RNA exosome to replicate and link defects in this machinery to neurodegeneration in rare genetic cases.
2016—First HIV+ to HIV+ organ transplant in New York State performed by Sander Florman, MD, and Susan Lerner, MD.
2016—Working with an international team, Mount Sinai researchers are the first to demonstrate the ability to reverse cardiac fibrosis in heart failure models by targeting a specific gene.
2016—Scientists publish first study to suggest that Alzheimer’s disease pathology increases susceptibility to diabetes due to impaired insulin signaling in the hypothalamus.
2016—A postdoctoral scientist and others publish a study that is the first to identify and validate the gene networks at play across brain circuits, showing that manipulating their activity alters the activity of brain cells and, ultimately, depression behavior.
2016—Researchers find that reversing impaired kidney function in diabetics may be possible with the ketogenic diet; the study is the first to show that a dietary intervention alone is enough to reverse this serious complication of diabetes.
2016—Mount Sinai researchers use PET scans to image tau buildup in a living former NFL player’s brain, marking the first in vivo detection of chronic traumatic encephalopathy-specific patterns.
2016—In a first-of-its-kind study, Mount Sinai ophthalmologists use optical coherence tomography angiography to detect early glaucoma by identifying distinct vascular patterns and reduced eye blood flow.
2016—Researchers in Dermatology identify the skin phenotype of pediatric atopic dermatitis—a finding that challenges the notion of filaggrin's central role in disease elicitation and instigation of the atopic march.
2015—Mount Sinai implants the responsive neurostimulation system in the youngest patients to date, pioneering its use in children with complex epilepsy syndromes.
2015—Kidney Stone Center opens for advanced and preventive care.
2015—Scientists find a first-in-class small molecule drug candidate, N106, which was able to improve the pumping ability of heart muscle cells.
2015—Surgeons in Urology perform the first successful robotic treatment for chyluria reported in the literature.
2015—Researchers in Genetics demonstrate for the first time that the microbiome of newborn babies delivered via cesarean section can be partially restored to resemble that of vaginally delivered infants.
2015—The Department of Urology is the first in the world to perform gold nanoparticle prostate cancer ablation.
2015—Scientists in Psychiatry provide the first demonstration in humans of transmission of pre-conception stress effects resulting in epigenetic changes in both the exposed parents and their offspring.
2015—Scientists from the Translational Molecular Imaging Institute at the Icahn School of Medicine are the first team to develop and begin clinical trials for the application and use of High Field 7T MRI imaging in the planning and operative guidance in complex endoscopic skull base surgery.
2014—Vivek Reddy, MD, implants the United States' first miniature-sized, leadless cardiac pacemaker directly inside a patient's heart without surgery.
2014—Universal flu vaccine developed for NIH trials by Peter Palese, PhD.
2014—Mount Sinai researchers show that ketamine can reverse suicidal ideation quickly.
2014—Mount Sinai scientists show that brain insulin signaling regulates branched-chain amino acids levels via liver metabolism, revealing a potential brain-based trigger for diabetes.
2014—Mount Sinai is first in the United States to use the FDA-approved Lutonix® drug-coated balloon catheter to open blocked arteries in the leg. A team led by researchers at the Icahn School proves that atopic dermatitis (eczema) is an immune-drive (autoimmune) disease at the molecular level.
2014—Mount Sinai scientists discover that active B-catenin in the brain promotes resilience to stress, while its deficiency is linked to depression in both humans and mice.
2013—The Mount Sinai Health System is formed through the merger of the Mount Sinai Medical Center and Continuum Health Partners, creating an integrated health care network across New York City.
2013—Mount Sinai researchers for the first time identify a small-viral RNA (svRNA) that is integral to the switch from transcription to replication.
2013—Researchers from the Icahn School of Medicine at Mount Sinai, in collaboration with other institutions, announce the discovery of the GNAL gene (Gαolf) as a new genetic basis for primary torsion dystonia.
2013—Gustave L. Levy Stroke Unit earns certification as Comprehensive Stroke Center.
2013—Mount Sinai develops the first gene test to identify cirrhosis patients at highest risk for liver cancer and predict recurrence after tumor removal.In a first-of its-kind study, researchers from the Seaver Autism Center for Research and Treatmentreveal the severity of intellectual, motor, and speech impairments Phelan-McDermid syndrome, a subtype of autism.
2013—Mount Sinai scientists identify an epigenetic link between diabetes and dementia, showing altered regulation of synaptic proteins may raise dementia risk.Mount Sinai doctors perform the first liver transplant in the United States for a patient with acute intermittent porphyria.
2013—Researchers make the first finding that small deletions impacting one or two genes appear to be common in autism, and that these deletions contribute to the risk of development of this disorder.
2012—FREEDOM trial shows coronary artery bypass grafting superior to angioplasty in diabetics with coronary artery disease.
2012—Five Crohn’s disease gene mutations found in Ashkenazi Jewish population.
2012—Mount Sinai scientists use a fruit fly cancer model to pioneer whole-animal screening for drug discovery, introducing the novel concept of an “anti-target.”
2012—Jeffrey W. Olin, DO, authors study that describes symptoms and severity offibromuscular dysplasia.
2012—In collaboration with an international group of colleagues, discovered five new genetic mutations associated with Crohn’s disease in Jews of Eastern European descent. This marks the largest study to date and the first to discover the unique risk factors of Crohn’s disease in the Ashkenazi Jewish population. The researchers also found that some previously known risk factors are more potent in this population than non-Jews.
2012—Identified a protein kinase that plays a significant role in kidney fibrosis, a condition that results in kidney failure.
2011—Uncovered how a gene mutation causes Parkinson’s disease.
2011—Identified differences in disease progression in two subtypes of multiple sclerosis.
2010—First human gene therapy trial for SERCA2a in heart failure succeeds.
2010—Standard definitions for bleeding in cardiovascular trials established by Roxana Mehran, MD.
2010—Presented research showing that the World Trade Center collapse caused potentially dangerous heart problems to first responders.
2010—Performed the first U.S. implantation of a new device for aortic stenosis.
2009—Carpentier-Edwards Physio II mitral valve ring is implanted by David Adams, MD, the first such procedure in the United States.
2009—Discovered potential link between rare blood cancer and environmental contaminants.
2008—Laser robotic head and neck cancer surgery implemented.
2008—Meng Law, MD, and colleagues from other institutions describe a new way to track brain tumor development and progression by measuring cerebral blood volume, which they showed was an accurate predictor of tumor malignancy; first noninvasive way to do it.
2007—Developed an advanced imaging technique to capture the movement of the microdomains of leukocytes, or white blood cells.
2007—Proved why influenza spreads most rapidly in the cold, dry air of winter, and showed that it can be spread just in the air, without coughing, sneezing, or physical contact.
2006—FluMist vaccine is developed using plasmid rescue tech by Adolfo García-Sastre, PhD, and Peter Palese, PhD.
2006—Identified three proteins found in significantly lower concentration in the cerebrospinal fluid of patients with amyotrophic lateral sclerosis than in healthy individuals.
2006—Discovered a gene in the brain—OLIG2—that may play a causal role in the development of schizophrenia.
2005—1918 flu virus reconstructed by Adolfo García-Sastre, PhD, and colleagues for modern research.
2005—Performed the first successful composite tracheal transplant, using a method developed at Mount Sinai that allows patients to breathe and speak without a tracheotomy. It is a composite of a donor trachea with the patient’s own tracheal linings.
2004—Mount Sinai nurses achieve Magnet® designation for nursing excellence.
2004—Identified the first common gene variant linked to autism.
2003—Fabrazyme is approved by the FDA to treat Fabry disease, developed by Robert Desnick, PhD, MD, David Bishop, PhD, and Yiannis Ioannou, PhD.
2001—Bruce Gelb, MD, discovers first gene for RASopathies (e.g., Noonan syndrome).
2001—Discovered the gene that is defective in most cases of prostate cancer.
2001—Developed a novel isothermal DNA amplification method with an amplification mechanism quite different from conventional polymerase chain reaction (PCR), resulting in an exponential amplification that distinguishes itself from the previously described nonexponential rolling circle amplification.
2000—Along with Case Western Reserve University School of Medicine, determined that HIV-associated nephropathy was caused by HIV-1 infection of kidney epithelial cells. This established that the best treatment for HIV+ patients in renal failure is antiretroviral treatment.
2000—Became the first to use black blood magnetic resonance imaging (BB-MR) to image the human coronary artery lumen.
1999—First multivisceral transplant in New York State is performed by Thomas Fishbein, MD.
1999—Center to Advance Palliative Care is established—drives U.S. palliative care adoption.
1998—Stuart Aaronson, MD, develops palifermin, the first approved treatment for mucositis.
1996—Identified a gene for a rare bone-thickening disease, pycnodysostosis, which causes dwarfism.
1995—Deep brain stimulation is used for Parkinson’s disease for the first time in the New York region.
1995—Developed an ultrasound-guided technique to insert radioactive seeds into the prostate to treat prostate cancer.
1993—First pediatric living donor liver transplant in New York State performed.
1992—John Eng, MD, discovers exendin-4, paving the way for GLP-1 receptor agonist drugs used in diabetes treatment and weight loss.
1992—Minimally invasive abdominal aortic aneurysm repair performed by Michael Marin, MD.
1992—First endovascular thoracic aneurysm surgery performed.
1991—Francesco Ramirez, DSc, discovers the gene for Marfan’s syndrome.
1991—In conjunction with the University of California, Irvine, College of Medicine, identified a marker for premature birth—the presence of cervicovaginal fetal fibronectin in the second and third trimesters of pregnancy.
1990—Global endometrial ablation via thermal balloon is developed.
1988—Charles Miller, MD, performs New York State’s first liver transplant.
1988—First use of colchicine to treat ulcerative colitis is published.
1988—Gustave L. Levy Acute Stroke Unit opens—the first of its kind in New York State.
1988—Demonstrated how asbestos causes cancerous changes in cellular DNA.
1987—Along with the Yale University School of Medicine, isolated and cloned a structural gene for human tissue factor.
1986—Performed the first blood transfusion into the vein of an unborn fetus.
1986—Developed an in vitro fertilization technique called zona drilling to help sperm cells penetrate egg cells.
1985 to 1933
1985—Provided the first direct evidence of the involvement of dopamine in schizophrenia.
1984—The Mount Sinai School of Medicine pioneers the use of simulated patients to assess clinical skills, leading to the establishment of The Morchand Center for Clinical Competence.
1983—Kenneth Davis, MD, leads development of cholinesterase inhibitors for Alzheimer’s disease.
1982—First academic geriatrics department in the United States is established at the Mount Sinai School of Medicine (now the Icahn School of Medicine at Mount Sinai).
1981—Daniel Present, MD, demonstrates the efficacy of mercaptopurine for Crohn’s disease.
1981—Discovered the proteasome (multicatalytic protease), the major regulated mechanism for protein degradation in the cell.
1977—Rosalyn Yalow, PhD, wins Nobel Prize for developing the radioimmunoassay technique for measuring hormone concentrations in bodily fluids, with early work by Solomon Berson, MD.
1977—Mapped the influenza virus genome.
1977—Platinum-based chemotherapy is used for the first time in the United States by Howard Bruckner, MD.
1971—Discovered that dimethyl sulfoxide could induce cancer cells to progress or differentiate to a normal pattern of development.
1969—Developed an influenza vaccine—the first genetically engineered vaccine.
1968—Confirmed multiple-factor causation of human cancer through work done on increased incidence of cancer among asbestos workers who smoked.
1964—Established etiologic link between asbestos and cancer.
1963—Became the first to use a sequential combination regimen of chemotherapy for adjuvant treatment of breast cancer.
1963—Provided the first description of superior limbic keratoconjunctivitis, now called Theodore's superior limbic keratoconjunctivitis (Theodore's SLK).
1962—Richard Rosenfield, MD, establishes Rh blood group system nomenclature.
1962—Became the first to use a sequential combination regimen of chemotherapy for adjuvant treatment of ovarian cancer.
1960—Published the first description of postperfusion syndrome after open-heart surgery.
1960—Performed the first radioimmunoassay of a hormone—a test capable of estimating nonogram or even picogram quantities.
1959—Developed radioimmunoassay.
1959—Created polyacrylamide gel electrophoresis for separating proteins.
1956—Classified transient circulatory disturbance of the brain, which came to be known as transient global ischemia.
1956—Developed and standardized the latex fixation test for the diagnosis of rheumatoid arthritis.
1952—Acid secretion inhibition via enzyme activity is discovered.
1952—Perfected and reintroduced surgery for the mobilization of the stapes.
1951—Became the first to perform closed mitral valve commissurotomy.
1950—Developed a portable kidney dialysis machine.
1950—Published first description of familial lipoprotein deficiency, known as Bassen-Kornzweig syndrome or abetalipoproteinemia.
1949—Published first description of allergic granulomatosis (Churg-Strauss syndrome).
1949—First identification and published description of Bassen-Kornzweig syndrome.
1947—Performed the first kidney dialysis in the United States, using a Kolff artificial kidney.
1944—Inhibited tumor growth by using a folic acid concentrate.
1942—Published the first description of collagen disease.
1940—Published the first description of eosinophilic granuloma of bone as a distinct entity.
1938—Hospital blood bank established and modeled nationwide.
1935—Published the first description of the vascular lesions in lupus.
1934—Described the first clinically applicable method for measuring the circulation time to the right heart.
1933—Published the first description of a total pneumonectomy in the United States.
1933—Introduced Hippuran as a radio-opaque medium.
1932 to 1887
1932—Published the first description of regional enteritis—an inflammatory disease of the intestine, now known as Crohn's disease.
1932—Established bronchial adenoma as a clinical and anatomic entity.
1932—Described and gave name to bronchopulmonary segments, a hitherto unnoticed feature of the pulmonary lobe.
1931—First Department of Intravenous Therapy in the United States established.
1931—Coined the term premenstrual syndrome.
1930—Published the first textbook in the United States on pediatric urology.
1929—Developed the first cardiac stress test known as the Master Two-Step.
1929—Introduced Uroselectan (Iopax) as the first radio-opaque media for visualization of the urinary tract.
1928—Published work on "Shwartzman Phenomenon"— a necrotic reaction to filtrates containing endotoxin of gram-negative bacteria.
1926—Developed test to measure estrogen levels in circulating blood.
1926—Described pulmonary hypertension as a separate clinical entity.
1925—Published the first description of hemolytic thrombocytopenic purpura (Moschcowitz disease).
1925—Published the first textbook in the United States on thoracic surgery.
1925—Published description of a new lymphatic system disease, later expanded by Douglas Symmers's work, later known as Brill-Symmers disease and then nodular lymphoma.
1924—Published description of atypical verrucous endocarditis, Libman-Sacks disease.
1923—Became the first in the United States to publish on gastrectomy for duodenal ulcers.
1920—Became the first to publish on gastrectomy in the United States for peptic ulcer disease.
1919—Introduced the use of peruterine insufflation of the fallopian tubes for the diagnosis and treatment of sterility in women (Rubin test.
1919—Performed experimental transmission of encephalitis lethargica.
1917—Described idiopathic nephrotic syndrome (Epstein's syndrome)—the cause of swelling in Bright's disease.
1915—Described the minimum amount of citrate required to prevent blood from clotting, making indirect transfusion possible and practical, and allowing blood to be stored for later transfusion. This paved the way for modern blood banking.
1914—Invented the first modern electric ophthalmoscope.
1914—Published the first textbook in the field of geriatrics.
1914—Pioneered salpingography—the x-ray visualization of the uterine tubes with radio-opaque substance.
1914—Performed the first pulmonary lobectomy for inflammatory disease.
1911—Developed the first cystoscope for children.
1910—Charles Elsberg, MD, develops positive-pressure anesthesia for thoracic surgery.
1910—The U.S.’s first continuous Department of Physical Medicine and Rehabilitation is founded.
1910—Identified endemic form of typhus fever (Brill's disease).
1910—Reported on a method of destroying benign tumors of the urinary bladder using electric current (fulguration).
1910—Developed the first practical positive pressure anesthesia technique (endotrachial anesthesia).
1910—Discovered that Strep. endocarditis is the most common cause of subacute bacterial endocarditis.
1910—Performed the first bypass and resective surgery for inflammatory colon disease.
1908—Published the first comprehensive report of clinical and pathological aspects of thrombo-angiitis obliterans (Buerger's disease)—a disease of the blood vessel walls that may result in gangrene.
1908—Published the first mention of using a blood test for compatibility before human blood transfusion. Became the first to note that blood groups are inherited according to Mendel's Law. Showed that group O blood could be given to group A and B patients, establishing the concept of the universal donor.
1904—The 456-bed, 10-pavilion Mount Sinai Hospital is dedicated on Fifth Avenue at 100th Street, marking a significant expansion to accommodate growing patient needs.
1901—Performed the first successful abdominal colectomy for colitis in the United States.
1892—Performed the first successful mastoidectomy in the United States.
1888—Published the first book in the United States on aseptic and antiseptic principles. This was also the first US medical textbook to use halftone photographs.
1887—Published the first description in the United States of condition later known as Tay-Sachs disease.